Fecal incontinence is a condition that affects millions of people worldwide. It can be a distressing and embarrassing problem that significantly impacts a person’s quality of life. In order to fully understand fecal incontinence and its causes, it is important to first define what it is and explore its prevalence in the population.
Defining Fecal Incontinence
Fecal incontinence, also known as bowel incontinence, refers to the involuntary leakage of stool from the rectum. It can range from occasional leakage of small amounts of stool to a complete loss of bowel control. This loss of control can occur with solid, liquid, or gas stool. While fecal incontinence can occur at any age, it is more commonly seen in older adults.
The Prevalence of Fecal Incontinence
The prevalence of fecal incontinence varies depending on the population studied. However, research suggests that it affects around 4-7% of the general population, with higher rates reported in nursing home residents and individuals with neurological conditions. Despite its frequency, many individuals suffer in silence and do not seek medical help due to embarrassment or lack of awareness about available treatments.
Living with fecal incontinence can be challenging, both physically and emotionally. The fear of accidents and the constant need to be near a bathroom can significantly impact a person’s quality of life. It can lead to social isolation, anxiety, and depression. Therefore, it is essential to raise awareness about this condition and encourage open discussions to reduce the stigma associated with it.
Furthermore, understanding the risk factors associated with fecal incontinence can help identify individuals who may be more susceptible to developing the condition. Some common risk factors include:
- Advanced age
- Female gender
- Pregnancy and childbirth
- Chronic constipation
- Neurological disorders, such as multiple sclerosis or spinal cord injuries
- Pelvic floor muscle dysfunction
- Prior rectal surgery
By recognizing these risk factors, healthcare professionals can provide targeted interventions and preventive measures to reduce the incidence of fecal incontinence.
Symptoms and Diagnosis
Fecal incontinence can manifest in different ways and may include the following symptoms:
- Uncontrolled passage of stool
- Inability to control gas
- Frequent urge to have a bowel movement
- Constipation
- Diarrhea
These symptoms can significantly impact the individual’s daily activities and emotional well-being. It is crucial to consult with a healthcare professional if experiencing any of these symptoms to receive an accurate diagnosis and appropriate treatment plan.
When diagnosing fecal incontinence, healthcare professionals may perform various tests and evaluations. These can include:
- Medical history review
- Physical examination, including a rectal examination
- Anorectal manometry to assess the strength and coordination of the anal sphincter muscles
- Anorectal ultrasound to evaluate the anatomy and function of the rectum and anal sphincter
- Proctography or defecography to assess the rectal and pelvic floor function during defecation
- Endoscopy to rule out any structural abnormalities or inflammation in the gastrointestinal tract
These diagnostic tests help healthcare professionals determine the underlying cause of fecal incontinence and develop an individualized treatment plan. Treatment options may include dietary modifications, medications, pelvic floor exercises, biofeedback therapy, and in severe cases, surgical interventions.
Overall, fecal incontinence is a complex condition that can significantly impact an individual’s quality of life. By increasing awareness, promoting open discussions, and providing appropriate medical interventions, we can support those affected by fecal incontinence and help them regain control over their lives.
The Parasympathetic Nervous System Explained
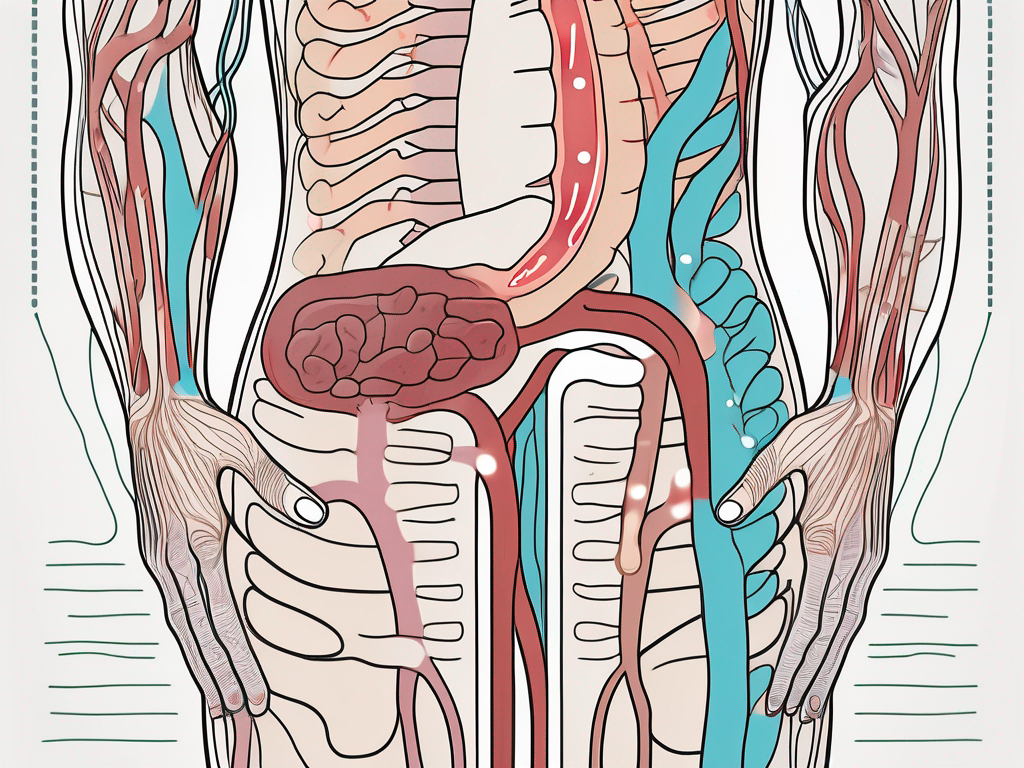
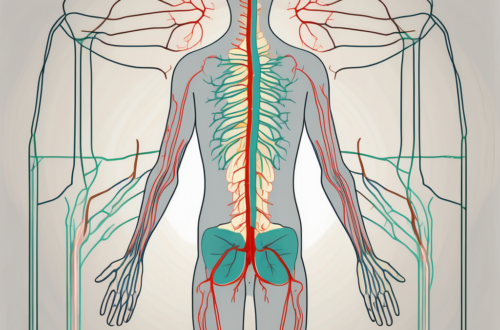
The parasympathetic nervous system is a vital component of the autonomic nervous system, which controls involuntary bodily functions. It works in opposition to the sympathetic nervous system, which is responsible for the body’s fight-or-flight response. The parasympathetic nervous system, on the other hand, promotes rest, relaxation, and digestion.
One of the key functions of the parasympathetic nervous system is its role in regulating bowel control. This intricate system orchestrates the complex process of digestion, ensuring that nutrients are properly absorbed and waste is efficiently eliminated.
Role of the Parasympathetic Nervous System in Bowel Control
When the parasympathetic nervous system is activated, it sends signals to the digestive organs, including the intestines and rectum. These signals stimulate the muscles in the intestine, promoting contraction and the movement of stool through the digestive tract. At the same time, it also relaxes the muscles in the rectum, allowing for the passage of stool during bowel movements.
Imagine a well-choreographed dance, where the parasympathetic nervous system acts as the conductor, coordinating the smooth and efficient movement of stool through the digestive system. Without this intricate coordination, the process of digestion would be disrupted, leading to various gastrointestinal issues.
How Nerve Damage Occurs
Unfortunately, the parasympathetic nervous system can be susceptible to damage, which can disrupt the normal functioning of the bowel. Nerve damage affecting this system can occur due to various factors, including:
- Childbirth trauma: The intense pressure exerted on the pelvic region during childbirth can sometimes cause damage to the nerves involved in bowel control.
- Rectal surgery: Surgical procedures involving the rectum can inadvertently damage the parasympathetic nerves, leading to bowel control issues.
- Inflammatory bowel disease: Conditions such as Crohn’s disease and ulcerative colitis can cause chronic inflammation in the digestive tract, potentially affecting the parasympathetic nervous system.
- Neurological conditions: Certain neurological conditions, such as multiple sclerosis or spinal cord injury, can damage the nerves responsible for bowel control, including those within the parasympathetic nervous system.
Understanding the connection between parasympathetic nerve injury and fecal incontinence is crucial in exploring effective treatment options. By identifying the underlying cause of the nerve damage, healthcare professionals can develop targeted interventions to alleviate symptoms and improve quality of life for individuals affected by bowel control issues.
Parasympathetic Nerve Injury and Fecal Incontinence
When the parasympathetic nerves that control bowel function are damaged, it can lead to fecal incontinence. The severity of incontinence can vary depending on the extent and location of the nerve injury.
Fecal incontinence is a distressing condition that can significantly impact a person’s quality of life. It is characterized by the involuntary loss of stool, which can occur at any time, including during physical activities or even while sleeping. The embarrassment and social stigma associated with fecal incontinence can lead to feelings of isolation and depression.
The Connection Between Nerve Injury and Incontinence
The parasympathetic nerves are responsible for signaling the muscles in the rectum to relax during defecation. This coordinated relaxation allows for the smooth passage of stool through the rectum and anus. When these nerves are damaged, the coordination between muscle relaxation and contraction is disrupted, leading to bowel control problems.
Damage to the parasympathetic nerves can occur due to various reasons, such as trauma, surgery, or certain medical conditions. Injuries to the lower spine, pelvic region, or rectum can directly affect the parasympathetic nerves, impairing their ability to transmit signals effectively.
Moreover, certain medical conditions, such as diabetes, multiple sclerosis, or spinal cord injuries, can also contribute to parasympathetic nerve damage. These conditions can cause inflammation or compression of the nerves, disrupting their normal functioning.
Risk Factors for Nerve Injury
Several factors can increase the risk of parasympathetic nerve injury and subsequent fecal incontinence. These include:
- Advanced age: As we age, the nerves in our body may become more vulnerable to damage, increasing the risk of nerve injury and subsequent fecal incontinence.
- Childbirth: The process of childbirth can put significant strain on the pelvic floor muscles and nerves, potentially leading to nerve damage and bowel control problems.
- Obesity: Excess weight can exert pressure on the pelvic region, potentially damaging the parasympathetic nerves and causing fecal incontinence.
- Prolonged constipation: Chronic constipation can lead to increased pressure in the rectum, which can strain and damage the parasympathetic nerves over time.
- Prior pelvic surgery: Surgical procedures in the pelvic region, such as those for treating colorectal conditions or gynecological issues, can inadvertently damage the parasympathetic nerves, leading to fecal incontinence.
It is important to note that while these risk factors may increase the likelihood of developing fecal incontinence, they do not guarantee the occurrence of nerve injury. Each individual’s case is unique, and consulting with a healthcare professional is essential for an accurate assessment of the situation.
Effective management of fecal incontinence requires a comprehensive approach that addresses both the physical and emotional aspects of the condition. Treatment options may include dietary modifications, pelvic floor exercises, medications, and in some cases, surgical interventions. Additionally, counseling and support groups can provide individuals with the necessary emotional support and coping strategies to navigate the challenges associated with fecal incontinence.
Treatment Options for Fecal Incontinence
The treatment of fecal incontinence depends on the underlying cause and the severity of the condition. It is crucial to consult with a healthcare professional to determine the most appropriate treatment plan.
Fecal incontinence, also known as bowel incontinence, is a condition that can significantly impact a person’s quality of life. It can cause embarrassment, social isolation, and a loss of independence. However, there are various treatment options available to manage and improve symptoms.
Non-Surgical Treatments
Non-surgical treatments for fecal incontinence may include:
- Dietary modifications: Adjusting the intake of certain foods to regulate bowel movements
- Medications: Prescribed medications to regulate bowel function and control symptoms
- Bowel training: Establishing a regular schedule for bowel movements to aid in control
- Pelvic floor exercises: Strengthening the muscles of the pelvic floor to improve control
These non-surgical options can often provide relief and improve symptoms. Dietary modifications, for example, may involve increasing fiber intake to promote regular bowel movements and avoiding trigger foods that can exacerbate symptoms. Medications can help regulate bowel function and reduce the frequency and urgency of bowel movements. Bowel training involves establishing a routine and sticking to it, which can help the body develop a predictable pattern of bowel movements. Pelvic floor exercises, such as Kegels, can strengthen the muscles that control bowel movements and improve overall control.
It is important to note that the effectiveness of each treatment may vary from person to person. A healthcare professional can help tailor the approach to individual needs, taking into account factors such as the underlying cause of fecal incontinence, overall health, and lifestyle.
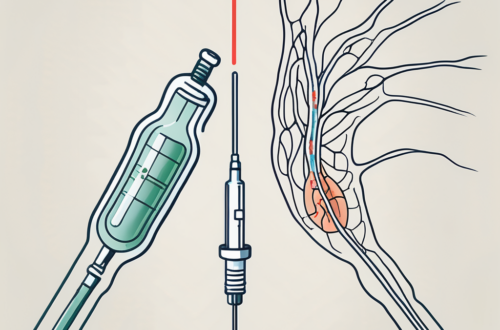
Surgical Treatments
In some cases, surgical intervention may be necessary to manage fecal incontinence. Surgical treatments can include procedures such as:
- Sphincter repair: Restoring the integrity and function of the anal sphincter muscles
- Neuromodulation: Stimulating the nerves that control bowel function to improve control
- Bowel diversion: Creating an alternate route for stool elimination
Surgical interventions are typically considered when non-surgical treatments have not provided sufficient relief or when the underlying cause of fecal incontinence necessitates surgical intervention. Sphincter repair surgery aims to restore the strength and coordination of the anal sphincter muscles, which play a crucial role in maintaining continence. Neuromodulation involves the use of electrical stimulation to modulate the nerves that control bowel function, helping to improve control. Bowel diversion surgery creates an alternative route for stool elimination, bypassing the rectum and anus altogether.
It is important to discuss the potential risks, benefits, and expected outcomes of surgical treatments with a healthcare professional. They can provide guidance and help determine if surgery is the most appropriate option based on individual circumstances.
In conclusion, fecal incontinence can be managed through a combination of non-surgical and surgical treatments. The choice of treatment depends on the underlying cause, severity of symptoms, and individual factors. Consulting with a healthcare professional is essential to develop a personalized treatment plan that addresses the specific needs and goals of each individual.
Living with Fecal Incontinence
Coping with fecal incontinence can be challenging, both physically and emotionally. However, there are strategies and support available to help individuals manage the condition and maintain their quality of life.
Fecal incontinence, also known as bowel incontinence, is the inability to control bowel movements, resulting in involuntary leakage of stool. This condition can be caused by a variety of factors, including muscle or nerve damage, certain medical conditions, or even certain medications. It can significantly impact a person’s daily life, leading to embarrassment, social isolation, and a decreased quality of life.
Lifestyle Adjustments
Implementing certain lifestyle adjustments can greatly improve symptoms and overall well-being. These may include:
- Establishing a regular bowel routine: Creating a consistent schedule for bowel movements can help regulate the digestive system and reduce the occurrence of accidents.
- Practicing good hygiene and using appropriate products: Proper hygiene is essential in managing fecal incontinence. This may involve using gentle cleansers, wipes, or bidets to keep the anal area clean and prevent skin irritation.
- Dietary modifications: Making changes to your diet can play a significant role in managing fecal incontinence. Increasing fiber intake can help regulate bowel movements, while staying hydrated ensures the stool remains soft and easier to control.
- Using protective measures: To minimize the impact of accidents, individuals can use absorbent pads or garments specifically designed for fecal incontinence. These products provide an extra layer of protection and help maintain dignity and confidence.
By incorporating these adjustments into daily life, individuals can regain control and minimize the impact of fecal incontinence on their daily activities.
Psychological Impact and Support
Fecal incontinence can have a significant psychological impact on individuals. The fear of accidents, embarrassment, and the constant worry about odor can lead to anxiety, depression, and a decreased self-esteem. It is important to seek emotional support from healthcare professionals or support groups.
Healthcare professionals who specialize in fecal incontinence can provide valuable guidance, advice, and a safe space to discuss concerns and experiences. They can help individuals understand the underlying causes of their condition, explore treatment options, and develop coping strategies. Support groups can also be an excellent source of encouragement, as individuals can connect with others who are going through similar experiences.
In conclusion, living with fecal incontinence can be challenging, but it is not a condition that individuals have to face alone. Understanding the lifestyle adjustments that can be made and seeking emotional support are crucial steps in managing this condition. With proper management and support, individuals with fecal incontinence can regain control, improve their overall quality of life, and find the confidence to engage in activities they enjoy.