The human body is a remarkable and complex system, composed of various organs and systems that work together to ensure our survival and well-being. One crucial component of this intricate network is the nervous system, which plays a vital role in controlling many bodily functions. Among these functions is the regulation of the bladder, a process that relies on a specific nerve known as the parasympathetic nerve. In this article, we will delve into the fascinating world of the parasympathetic nervous system and explore its involvement in bladder innervation.
Understanding the Parasympathetic Nervous System
The parasympathetic nervous system is one of the two main divisions of the autonomic nervous system, responsible for regulating involuntary bodily processes. It opposes the actions of the sympathetic nervous system, which governs the body’s “fight or flight” response. Instead, the parasympathetic nervous system promotes a state of rest, relaxation, and digestion.
When we think about the parasympathetic nervous system, it’s essential to understand its role in maintaining the body’s internal balance, known as homeostasis. This intricate system plays a crucial part in ensuring that our bodily functions work harmoniously together.
The Role of the Parasympathetic Nervous System
Primarily, the parasympathetic nervous system is responsible for stimulating certain organs and structures to maintain homeostasis. It controls various bodily functions, including heart rate, digestion, and urinary system activities such as bladder control.
Let’s dive deeper into the role of the parasympathetic nervous system in maintaining heart rate. When we are in a state of rest, the parasympathetic nervous system slows down our heart rate, ensuring that it beats at a steady pace. This allows our heart to efficiently pump blood throughout the body, providing oxygen and nutrients to all our organs and tissues.
Furthermore, the parasympathetic nervous system plays a vital role in digestion. When we sit down to enjoy a meal, this branch of the autonomic nervous system kicks into action. It stimulates the release of digestive enzymes, enhances the secretion of stomach acid, and promotes the rhythmic contractions of the gastrointestinal tract. All of these processes work together to break down food, absorb nutrients, and eliminate waste products.
Key Components of the Parasympathetic Nervous System
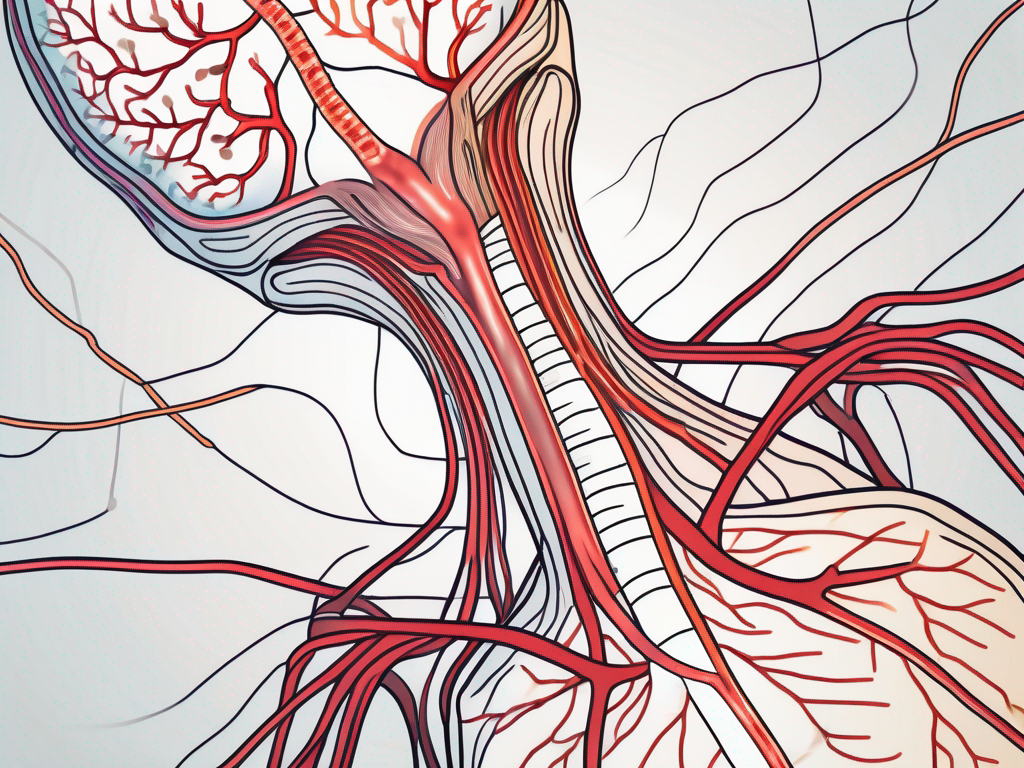
The parasympathetic nervous system consists of two main components: the cranial nerves and the sacral nerves. The cranial nerves originate from the brain, while the sacral nerves arise from the sacral region of the spinal cord. Both sets of nerves work together to innervate different organs and systems throughout the body.
Let’s explore the cranial nerves in more detail. There are twelve pairs of cranial nerves, each with its specific functions and innervations. For example, the vagus nerve, also known as cranial nerve X, is a major player in the parasympathetic nervous system. It innervates organs such as the heart, lungs, and digestive system, ensuring their proper functioning.
On the other hand, the sacral nerves, originating from the sacral region of the spinal cord, play a crucial role in innervating the pelvic organs. These nerves are responsible for controlling activities such as bladder control, sexual function, and bowel movements. Without the parasympathetic control provided by the sacral nerves, these essential bodily functions would be disrupted.
In conclusion, the parasympathetic nervous system is a fascinating and intricate part of our autonomic nervous system. Its role in maintaining homeostasis, regulating heart rate, promoting digestion, and controlling various bodily functions cannot be overstated. Understanding the parasympathetic nervous system allows us to appreciate the complexity of our bodies and the incredible mechanisms that keep us functioning optimally.
The Nervous System and the Bladder
The nerves that innervate the bladder play a vital role in its control and functionality. Through a complex interplay between the central and peripheral nervous systems, the bladder can store and eliminate urine efficiently.
The nervous system relies on intricate signaling pathways to regulate bladder function. When the bladder contains a certain volume of urine, sensory nerves communicate this information to the brain, which coordinates the appropriate response. Subsequently, signals are sent through the parasympathetic nervous system to stimulate the relaxation of the bladder’s detrusor muscle, allowing the bladder to fill with urine.
Conversely, when it is time to empty the bladder, the brain sends signals down the spinal cord, activating the parasympathetic nerves that trigger the contraction of the detrusor muscle and the relaxation of the urinary sphincter muscles. This coordinated action facilitates the voluntary expulsion of urine.
In addition to these primary functions, the nervous system also plays a role in modulating bladder sensation. Specialized nerve fibers called C-fibers transmit information about bladder fullness and pressure to the brain, allowing us to perceive the need to urinate. This sensory feedback loop is crucial for maintaining continence and preventing involuntary leakage.
Furthermore, the nervous system is involved in regulating the timing and frequency of bladder emptying. The brain’s control over the bladder extends to the coordination of the micturition reflex, which is the process by which the bladder contracts and the sphincter relaxes to initiate urination. This reflex is finely tuned by neural circuits in the spinal cord, ensuring that urination occurs at appropriate times and in a controlled manner.
The Impact of Nerve Damage on Bladder Control
However, just like any other system in the body, the nervous system is susceptible to damage or dysfunction. Nerve damage or injury can disrupt the delicate balance of bladder control, leading to various urinary disorders. Conditions such as neurogenic bladder, where nerve signals to the bladder are impaired, can result in problems with urine storage and elimination.
In cases of nerve damage, the communication between the bladder and the brain may be compromised. This can lead to a loss of sensation, making it difficult for individuals to perceive when their bladder is full or empty. As a result, they may experience urinary retention, where the bladder fails to empty completely, or urinary incontinence, where urine leaks involuntarily.
Nerve damage can also affect the coordination of the micturition reflex, causing problems with bladder emptying. In some cases, the detrusor muscle may become overactive, leading to a condition known as overactive bladder. This can result in frequent and urgent urination, as well as urinary urgency incontinence, where individuals experience leakage due to an uncontrollable urge to urinate.
On the other hand, nerve damage can also cause underactive bladder, where the detrusor muscle fails to contract effectively. This can lead to difficulties in initiating urination and incomplete bladder emptying.
Overall, the intricate relationship between the nervous system and the bladder highlights the importance of maintaining a healthy nervous system for optimal bladder function. By understanding the role of nerves in bladder control and the potential consequences of nerve damage, healthcare professionals can develop targeted interventions to help individuals manage and improve their bladder health.
The Pelvic Nerve: Innervation of the Bladder
One crucial nerve involved in bladder innervation is the pelvic nerve. It originates from the sacral region of the spinal cord and extends towards the pelvic organs, including the bladder.
The pelvic nerve, also known as the nervus pelvicus, is a complex network of nerve fibers that plays a pivotal role in the proper functioning of the bladder. It is part of the autonomic nervous system, which controls involuntary bodily functions.
Anatomy of the Pelvic Nerve
The pelvic nerve is a mixed nerve consisting of both sensory and motor fibers. Sensory fibers transmit information from the bladder to the brain, allowing for the perception of urinary sensations. These sensations can range from the feeling of a full bladder to the urge to urinate.
Motor fibers, on the other hand, control the contraction and relaxation of the bladder muscles. When the bladder needs to empty its contents, the motor fibers of the pelvic nerve stimulate the detrusor muscle, causing it to contract and expel urine through the urethra.
The pelvic nerve is not a single nerve but rather a collection of nerves that originate from the sacral region of the spinal cord. These nerves branch out and form a complex network that innervates various pelvic organs, including the bladder, uterus, and rectum.
The Pelvic Nerve’s Role in Bladder Function
The pelvic nerve serves as a vital conduit between the bladder and the central nervous system, ensuring effective communication and coordination between these two entities. When the bladder is full, the pelvic nerve relays this information to the brain, prompting the appropriate response for urine elimination.
When the bladder is empty, the sensory fibers of the pelvic nerve detect the absence of urine and send signals to the brain, indicating that there is no need for immediate urination. This feedback loop allows for the regulation of bladder function, preventing unnecessary and untimely urination.
In addition to its role in bladder function, the pelvic nerve also plays a crucial role in sexual function. It provides innervation to the genital organs, including the penis and clitoris, contributing to sexual arousal and orgasm.
Damage or dysfunction of the pelvic nerve can lead to various bladder problems, such as urinary incontinence or retention. Conditions such as pelvic nerve neuropathy or pelvic floor dysfunction can disrupt the normal functioning of the nerve, affecting bladder control and overall quality of life.
In conclusion, the pelvic nerve is a vital component of the bladder’s innervation. Its complex anatomy and role in bladder function highlight its importance in maintaining urinary continence and overall pelvic health.
Disorders Related to Bladder Innervation
Unfortunately, disorders related to bladder innervation can significantly impact an individual’s quality of life and well-being. Understanding these conditions is imperative for prompt diagnosis and appropriate management.
The bladder, a hollow organ located in the lower abdomen, plays a crucial role in the elimination of waste from the body. It relies on a complex network of nerves to coordinate its functions, including the storage and release of urine. When there is a disruption in the innervation of the bladder, various disorders can arise, leading to bothersome symptoms and complications.
Overactive Bladder and Nerve Dysfunction
An overactive bladder is a common condition characterized by a strong and sudden urge to urinate, sometimes resulting in urinary incontinence. While several factors can contribute to this condition, nerve dysfunction is often a significant underlying cause.
The nerves responsible for controlling the bladder’s contractions and relaxation may become hyperactive, sending frequent and inappropriate signals to the bladder muscles. This constant signaling can lead to an overactive bladder, causing individuals to experience an urgent need to urinate, even when the bladder is not full.
Furthermore, nerve dysfunction can disrupt the coordination between the bladder muscles and the urinary sphincter, the muscle responsible for holding urine in the bladder. This can result in episodes of urinary incontinence, where urine leaks involuntarily.
Seeking medical evaluation from a qualified healthcare professional is critical to determine the precise cause of an overactive bladder and receive proper treatment. Treatment options may include lifestyle modifications, bladder training exercises, medications, or in severe cases, surgical interventions.
Neurogenic Bladder: Causes and Symptoms
Neurogenic bladder refers to a loss of normal bladder function due to nerve damage or dysfunction. This condition can manifest as urinary incontinence, urinary retention (inability to empty the bladder completely), or a combination of both.
There are various underlying causes of neurogenic bladder, each with its own set of symptoms and management strategies. Spinal cord injuries, for example, can disrupt the communication between the bladder and the brain, leading to a loss of control over bladder function. Conditions like multiple sclerosis, a chronic autoimmune disease affecting the central nervous system, can also damage the nerves that innervate the bladder.
In addition to spinal cord injuries and multiple sclerosis, other conditions such as diabetes, stroke, Parkinson’s disease, and certain medications can also contribute to the development of neurogenic bladder.
Consulting with a healthcare provider is crucial to managing neurogenic bladder effectively. A thorough evaluation, including a detailed medical history, physical examination, and possibly additional tests, will help determine the underlying cause and guide the treatment approach. Treatment options may include medications to relax or stimulate the bladder muscles, intermittent catheterization to empty the bladder, or surgical interventions to improve bladder function.
Treatment Options for Bladder Innervation Disorders
Bladder innervation disorders can cause significant disruptions to a person’s quality of life. Fortunately, various treatment options are available to address these disorders and restore normal bladder function.
One of the primary treatment approaches for bladder innervation disorders is the use of medications. Pharmacological treatments, such as anticholinergic medications, can help manage conditions like overactive bladder. These medications work by relaxing the bladder muscles and reducing abnormal contractions. However, it is important to note that the suitability of these medications varies from person to person. Only a healthcare professional can determine the most appropriate treatment course based on an individual’s specific needs and medical history.
In addition to medications, surgical interventions may be necessary in certain cases. Procedures such as sacral neuromodulation or bladder augmentation can help improve bladder function and alleviate symptoms. Sacral neuromodulation involves the implantation of a device that delivers electrical impulses to the nerves that control the bladder, helping to regulate its function. On the other hand, bladder augmentation is a surgical procedure that increases the capacity of the bladder, reducing the frequency of urination and improving overall bladder control. However, it is important to note that these surgical options should be carefully considered and discussed with a qualified urologist or specialist.
Aside from medications and surgery, there are also non-invasive treatment options available for bladder innervation disorders. These include bladder training techniques, pelvic floor exercises, and lifestyle modifications. Bladder training involves gradually increasing the time between urination to improve bladder control. Pelvic floor exercises, such as Kegel exercises, can strengthen the muscles that support the bladder, leading to improved bladder function. Making certain lifestyle modifications, such as avoiding bladder irritants like caffeine and alcohol, can also help manage bladder innervation disorders.
In conclusion, understanding the role of the parasympathetic nervous system in bladder innervation is crucial for comprehending the complex mechanisms involved in bladder control. Nerve damage or dysfunction can significantly impact bladder function, leading to various urinary disorders. Seeking medical evaluation from healthcare professionals is essential for accurate diagnosis and appropriate treatment. With advancements in medical knowledge and technology, managing bladder innervation disorders is possible, allowing individuals to regain control and improve their overall quality of life.