The vagus parasympathetic nerve plays a crucial role in regulating various bodily functions. Understanding its anatomy, functions, and the connections it has with different systems in the body can provide valuable insights into overall health and well-being. In this article, we will explore the vagus nerve in detail, examining its anatomy, functions, its impact on the immune response, the brain-body connection, disorders related to the nerve, and future research directions.
Understanding the Vagus Parasympathetic Nerve
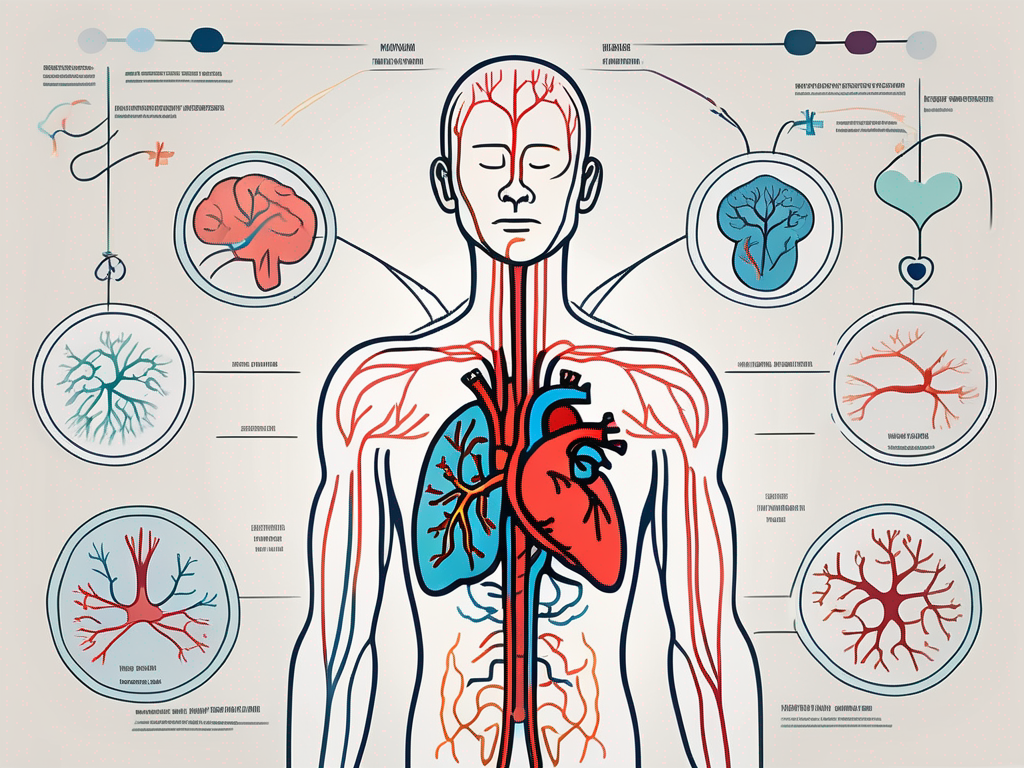
The vagus parasympathetic nerve, also known as the tenth cranial nerve, is a long and complex nerve that originates from the brainstem and extends down into various organs throughout the body. It is a major component of the parasympathetic nervous system, which is responsible for regulating the body’s rest and digest response.
The vagus nerve plays a crucial role in maintaining the body’s overall well-being. It is involved in a wide range of functions, including heart rate regulation, digestion, and even influencing our emotional state. Without the vagus nerve, our bodies would struggle to maintain balance and function optimally.
Anatomy and Location of the Vagus Nerve
The vagus nerve is the longest cranial nerve, and it originates from the medulla oblongata in the brainstem. From there, it extends down through the neck and chest, innervating various organs such as the heart, lungs, and digestive system. It has both sensory and motor fibers, allowing it to transmit information to and from the brain.
As the vagus nerve travels through the body, it branches out extensively, forming a complex network of fibers that reach almost every major organ. This extensive innervation allows the vagus nerve to have a profound influence on our bodily functions.
The Parasympathetic Nervous System: A Brief Overview
The vagus nerve is part of the parasympathetic nervous system, one of the two branches of the autonomic nervous system. The parasympathetic nervous system is responsible for promoting the body’s relaxation response, which helps conserve energy and maintain homeostasis. It counterbalances the sympathetic nervous system’s fight-or-flight response, allowing the body to conserve energy and prioritize restorative processes.
When the parasympathetic nervous system is activated, the vagus nerve releases acetylcholine, a neurotransmitter that slows down heart rate, increases digestive activity, and promotes a sense of calm and relaxation. This activation allows the body to divert resources towards essential functions such as digestion, tissue repair, and immune system regulation.
Interestingly, the vagus nerve also plays a role in our emotional well-being. It is connected to various brain regions involved in emotional processing, such as the amygdala and prefrontal cortex. This connection allows the vagus nerve to influence our mood and emotional responses, highlighting its importance beyond its role in regulating bodily functions.
In conclusion, the vagus parasympathetic nerve is a remarkable and intricate part of our nervous system. Its extensive reach and involvement in various bodily functions make it a vital component for maintaining overall health and well-being. Understanding the vagus nerve’s anatomy and its role in the parasympathetic nervous system provides valuable insights into the complexity of our bodies and the intricate mechanisms that keep us functioning optimally.
Functions of the Vagus Parasympathetic Nerve
The vagus nerve is involved in regulating various bodily functions, playing a key role in maintaining overall health and well-being.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and digestive system. This extensive network allows the vagus nerve to have a wide range of functions and influences on different bodily systems.
Role in Heart Rate Regulation
One of the crucial functions of the vagus nerve is its role in regulating heart rate. Through its connections with the heart, the vagus nerve helps control the heart’s rhythm and keeps it within a healthy range. It helps to slow down the heart rate during periods of rest and relaxation, promoting overall cardiac health.
Furthermore, the vagus nerve is responsible for the release of acetylcholine, a neurotransmitter that helps regulate heart rate. Acetylcholine acts as a natural pacemaker, slowing down the electrical impulses that control the heart’s contractions. This mechanism ensures that the heart beats at a steady and appropriate pace, preventing irregularities and maintaining cardiovascular stability.
Influence on Digestive System
The vagus nerve also plays a significant role in the functioning of the digestive system. It helps stimulate the release of digestive enzymes, enhances intestinal motility, and promotes the absorption of nutrients. Additionally, the vagus nerve helps facilitate communication between the gut and the brain, forming what is known as the gut-brain axis. This connection is crucial for maintaining a healthy digestive system.
When food enters the stomach, the vagus nerve sends signals to stimulate the release of gastric acid and digestive enzymes, aiding in the breakdown of food. It also helps regulate the movement of food through the digestive tract, ensuring efficient absorption of nutrients and elimination of waste. Moreover, the vagus nerve plays a role in signaling feelings of hunger and satiety, contributing to the regulation of appetite and body weight.
Impact on Respiratory System
In addition to its influence on the cardiovascular and digestive systems, the vagus nerve also has an impact on the respiratory system. It helps regulate the rate and depth of breathing, ensuring that the body receives an adequate supply of oxygen. The vagus nerve also plays a role in controlling the body’s response to carbon dioxide levels, helping to maintain proper respiratory function.
When the body detects an increase in carbon dioxide levels, the vagus nerve sends signals to stimulate the respiratory muscles, leading to deeper and more frequent breaths. This response helps expel excess carbon dioxide and replenish oxygen levels in the body. Conversely, when carbon dioxide levels decrease, the vagus nerve reduces the rate and depth of breathing, preventing hyperventilation and maintaining respiratory balance.
Moreover, the vagus nerve is involved in the regulation of the cough reflex, helping to clear the airways of irritants and maintain respiratory health. It also plays a role in controlling the diameter of the airways, ensuring optimal airflow and preventing respiratory conditions such as asthma.
The Vagus Nerve and the Immune Response
Recent research has shed light on the connection between the vagus nerve and the immune system, highlighting the nerve’s involvement in modulating inflammation.
The vagus nerve, also known as the tenth cranial nerve, is the longest and most complex of the cranial nerves. It originates in the brainstem and extends down to various organs in the body, including the heart, lungs, and digestive system. While traditionally known for its role in regulating heart rate and digestion, scientists have discovered that the vagus nerve also plays a crucial role in modulating the immune response.
Vagus Nerve Stimulation and Inflammation Reduction
Studies have shown that stimulating the vagus nerve through a technique called vagus nerve stimulation (VNS) can help reduce inflammation in the body. VNS involves delivering mild electrical impulses to the nerve, triggering a response that can inhibit excessive inflammation. This has potential therapeutic implications for various inflammatory conditions, although further research is needed to fully understand the mechanisms and develop targeted treatments.
One study conducted on rats found that VNS significantly reduced inflammation in the lungs, suggesting that this technique could be beneficial for respiratory conditions such as asthma or chronic obstructive pulmonary disease (COPD). Another study showed that VNS reduced inflammation in the gut, indicating its potential for treating inflammatory bowel diseases like Crohn’s disease and ulcerative colitis.
Furthermore, VNS has shown promise in reducing inflammation in the brain. Inflammation in the brain has been linked to various neurological disorders, including Alzheimer’s disease, Parkinson’s disease, and multiple sclerosis. By targeting the vagus nerve, researchers hope to develop novel therapies that can alleviate inflammation and potentially slow down the progression of these debilitating conditions.
The Cholinergic Anti-inflammatory Pathway
The vagus nerve’s influence on inflammation is partly mediated through what is known as the cholinergic anti-inflammatory pathway. This pathway involves the release of acetylcholine, a neurotransmitter, which dampens the production of pro-inflammatory molecules. By activating this pathway, the vagus nerve can help regulate the immune response and prevent excessive inflammation.
Acetylcholine acts as a signaling molecule that binds to specific receptors on immune cells, triggering a cascade of events that result in the suppression of inflammation. This anti-inflammatory effect is particularly important in preventing the immune system from overreacting to harmless stimuli, which can lead to chronic inflammation and tissue damage.
Interestingly, the cholinergic anti-inflammatory pathway is not only activated by VNS but can also be stimulated through non-invasive techniques such as deep breathing exercises and meditation. These techniques promote a state of relaxation and activate the parasympathetic nervous system, which includes the vagus nerve. By incorporating these practices into daily life, individuals may be able to enhance the natural anti-inflammatory capabilities of their vagus nerve and potentially reduce the risk of chronic inflammatory conditions.
In conclusion, the vagus nerve plays a crucial role in modulating the immune response and controlling inflammation throughout the body. Vagus nerve stimulation and the cholinergic anti-inflammatory pathway offer promising avenues for developing new treatments for inflammatory conditions. As researchers continue to unravel the complexities of this intricate connection, the potential for targeted therapies that harness the power of the vagus nerve to combat inflammation becomes increasingly exciting.
The Vagus Nerve and the Brain-Body Connection
The vagus nerve serves as a vital link between the brain and the rest of the body, facilitating communication and influencing various aspects of mental and physical health.
The vagus nerve, also known as the tenth cranial nerve, is the longest nerve in the body. It originates in the brainstem and branches out to innervate various organs, including the heart, lungs, digestive system, and even the muscles of the face and neck. This extensive network allows the vagus nerve to play a crucial role in regulating numerous bodily functions.
Vagus Nerve’s Role in Stress Response
One of the key functions of the vagus nerve is its involvement in the body’s response to stress. Through its connections with the brain, the vagus nerve helps regulate the release of stress hormones and modulates the stress response. When we encounter a stressful situation, the vagus nerve sends signals to the brain, triggering the release of stress hormones like cortisol and adrenaline. These hormones prepare the body for the “fight or flight” response, enabling us to react quickly and effectively.
However, the vagus nerve also plays a crucial role in the body’s ability to recover from stress. After the initial stress response, the vagus nerve helps activate the parasympathetic nervous system, which promotes relaxation and restores balance to the body. This process is known as the “rest and digest” response, and it is essential for maintaining overall well-being.
A healthy functioning vagus nerve is important for maintaining resilience and managing stress effectively. When the vagus nerve is functioning optimally, it helps regulate the stress response, allowing us to adapt and cope with challenging situations. On the other hand, when the vagus nerve is compromised or not functioning properly, it can lead to an overactive stress response, contributing to chronic stress and its associated health problems.
Impact on Mood and Mental Health
Research has also shown a relationship between the vagus nerve and mental health. The vagus nerve has been implicated in regulating mood, and abnormalities in vagal tone – the measure of vagus nerve activity – have been associated with conditions such as depression and anxiety.
Studies have found that individuals with higher vagal tone tend to have better emotional regulation and are more resilient to stress. On the other hand, low vagal tone has been linked to increased vulnerability to mood disorders and difficulties in managing emotions. This suggests that optimizing vagal tone and supporting vagus nerve health may have positive effects on mental well-being.
There are various techniques and practices that can help stimulate the vagus nerve and improve vagal tone. Deep breathing exercises, meditation, yoga, and even singing can all activate the vagus nerve and promote relaxation. Additionally, engaging in activities that promote social connection and positive emotions, such as spending time with loved ones or practicing gratitude, can also have a beneficial impact on vagal tone.
While the exact mechanisms underlying the relationship between the vagus nerve and mental health are still being explored, it is clear that this intricate connection plays a significant role in our overall well-being. By understanding the importance of the vagus nerve and taking steps to support its health, we can enhance our brain-body connection and promote better mental and physical health.
Disorders Related to the Vagus Parasympathetic Nerve
Despite its essential role in maintaining bodily functions, the vagus nerve can be affected by various disorders that can impact overall health and well-being.
The vagus nerve, also known as the tenth cranial nerve, is a crucial component of the parasympathetic nervous system. It plays a vital role in regulating many bodily functions, including heart rate, digestion, and inflammation. However, like any other part of the body, the vagus nerve is susceptible to dysfunction and disorders that can disrupt its normal functioning.
Vagus nerve dysfunction can manifest in a variety of ways, with symptoms ranging from digestive issues, heart rate irregularities, and difficulty swallowing to mood disturbances and chronic inflammation. These symptoms can significantly impact an individual’s quality of life and overall well-being.
One of the common causes of vagus nerve dysfunction is trauma. Physical injuries, such as car accidents or falls, can damage the nerve and disrupt its normal functioning. Infections, such as Lyme disease or viral infections, can also affect the vagus nerve and lead to dysfunction. Additionally, chronic diseases like diabetes or autoimmune disorders can contribute to vagus nerve disorders.
Furthermore, certain medications can have an adverse effect on the vagus nerve. Drugs that target the nervous system, such as antidepressants or antipsychotics, can interfere with the nerve’s ability to transmit signals effectively. It is crucial for individuals experiencing symptoms related to vagus nerve dysfunction to consult a healthcare professional for an accurate diagnosis and appropriate management strategies.
Treatment Options for Vagus Nerve Disorders
For individuals diagnosed with vagus nerve disorders, various treatment options may be available. The choice of treatment depends on the specific disorder and its underlying cause. In some cases, lifestyle modifications can be effective in managing symptoms. These modifications may include stress reduction techniques, such as meditation or yoga, as stress can exacerbate vagus nerve dysfunction.
Medications can also be prescribed to alleviate symptoms and improve the functioning of the vagus nerve. For example, medications that target heart rate irregularities or digestive issues can help regulate these bodily functions. In severe cases, surgical interventions may be necessary to repair or replace damaged portions of the vagus nerve.
It is important to note that each individual’s treatment plan should be tailored to their specific needs. Consulting with a healthcare professional who specializes in neurology or autonomic disorders is essential for proper diagnosis and the development of an effective treatment plan.
In conclusion, disorders related to the vagus parasympathetic nerve can have a significant impact on an individual’s health and well-being. Understanding the symptoms, causes, and treatment options for vagus nerve dysfunction is crucial for managing these disorders effectively. By seeking appropriate medical care and following a personalized treatment plan, individuals can improve their quality of life and minimize the impact of vagus nerve disorders.
Future Research Directions in Vagus Nerve Study
While much has been discovered about the vagus nerve, there are still many unexplored areas and potential therapeutic applications that require further investigation.
Potential Therapeutic Applications of Vagus Nerve Stimulation
Vagus nerve stimulation has shown promising results in reducing inflammation and managing various conditions, such as epilepsy and depression. Ongoing research aims to explore the potential therapeutic applications of VNS in other areas, such as chronic pain, autoimmune disorders, and neurodegenerative diseases. By further understanding the mechanisms and optimizing stimulation techniques, VNS may offer new treatment options for various conditions.
Unexplored Areas in Vagus Nerve Research
Despite significant progress in vagus nerve research, there are still many unanswered questions. Further exploration is needed to understand the specifics of the gut-brain axis, the effects of vagus nerve stimulation on different systems, and the intricacies of the cholinergic anti-inflammatory pathway. By delving deeper into these areas, researchers can uncover new insights into the role of the vagus nerve in regulating bodily functions and potential areas for therapeutic intervention.
In conclusion, the vagus parasympathetic nerve plays a vital role in regulating bodily functions and maintaining overall health and well-being. Its influence extends beyond the cardiovascular, digestive, and respiratory systems to include the immune response and the brain-body connection. Understanding the vagus nerve’s anatomy, functions, and associated disorders provides valuable insights into the intricate connections that govern our bodily processes. While many aspects of vagus nerve study have been explored, ongoing research continues to expand our knowledge, offering potential therapeutic applications and areas for future investigation. It is advisable to consult with a healthcare professional for accurate diagnosis, management, and treatment options related to vagus nerve disorders.