The pupillary function is a complex process that involves the interaction of several nerves and muscles in the eye. One such nerve that plays a crucial role in pupillary function is the parasympathetic nerve. In this article, we will explore the significance of the parasympathetic nerve in pupillary function and its implications in various eye disorders.
An Overview of the Parasympathetic Nervous System
Before delving into the role of the parasympathetic nerve in pupillary function, it is essential to understand the basics of the parasympathetic nervous system. The parasympathetic nervous system is one of the divisions of the autonomic nervous system, responsible for regulating various involuntary bodily functions. It works in opposition to the sympathetic nervous system, which controls the body’s fight-or-flight response.
The parasympathetic nervous system primarily functions to conserve energy and promote relaxation. It has a crucial role in controlling activities such as digestion, heart rate, and pupil constriction.
Key Components of the Parasympathetic Nervous System
The parasympathetic nervous system consists of various key components that work together to regulate bodily functions, including pupillary function. The main control center of this system is the cranial nerve known as the vagus nerve (CN X). The vagus nerve originates in the medulla oblongata and branches out to innervate multiple organs, including the heart, lungs, and eyes.
Other important components of the parasympathetic nervous system include the ciliary ganglion, which is responsible for controlling the focusing ability of the eye, and the Edinger-Westphal nucleus, which regulates pupillary constriction.
The ciliary ganglion is a small cluster of nerve cells located behind the eye. It receives signals from the brain via the vagus nerve and sends out commands to the muscles that control the shape of the lens in the eye. By adjusting the shape of the lens, the ciliary ganglion helps to focus incoming light onto the retina, allowing for clear vision.
The Edinger-Westphal nucleus, on the other hand, is a group of neurons located in the midbrain. It receives input from the visual cortex and sends signals to the ciliary ganglion, which in turn controls the size of the pupil. When the Edinger-Westphal nucleus is activated, it causes the circular muscles of the iris, known as the sphincter pupillae, to contract. This results in a decrease in the size of the pupil, allowing less light to enter the eye. Conversely, inhibition of the parasympathetic nervous system leads to pupillary dilation.
Functions of the Parasympathetic Nervous System
The parasympathetic nervous system exerts its effects through the release of a neurotransmitter called acetylcholine. This neurotransmitter binds to specific receptors in target tissues and initiates a cascade of events that lead to various physiological responses.
In the context of pupillary function, the parasympathetic nervous system plays a crucial role in pupillary constriction. When activated, it causes the sphincter pupillae muscles to contract, reducing the size of the pupil. This serves to protect the retina from excessive light exposure and helps to improve visual acuity in bright conditions.
Additionally, the parasympathetic nervous system is involved in regulating other bodily functions. For example, it stimulates the production of saliva, which aids in digestion. It also slows down the heart rate and promotes relaxation, allowing the body to conserve energy and recover from stress.
Furthermore, the parasympathetic nervous system is responsible for promoting peristalsis, the rhythmic contractions of the smooth muscles in the digestive tract that propel food along the gastrointestinal tract. It also stimulates the release of digestive enzymes and increases blood flow to the digestive organs, facilitating the process of digestion and absorption of nutrients.
Overall, the parasympathetic nervous system is a vital component of the autonomic nervous system, working in harmony with the sympathetic nervous system to maintain homeostasis and regulate various bodily functions. Its role in pupillary function is just one example of its intricate and essential functions in the human body.
The Parasympathetic Nerve and the Eye
To understand the role of the parasympathetic nerve in pupillary function, it is essential to explore the anatomy of the eye and its relevance to parasympathetic control.
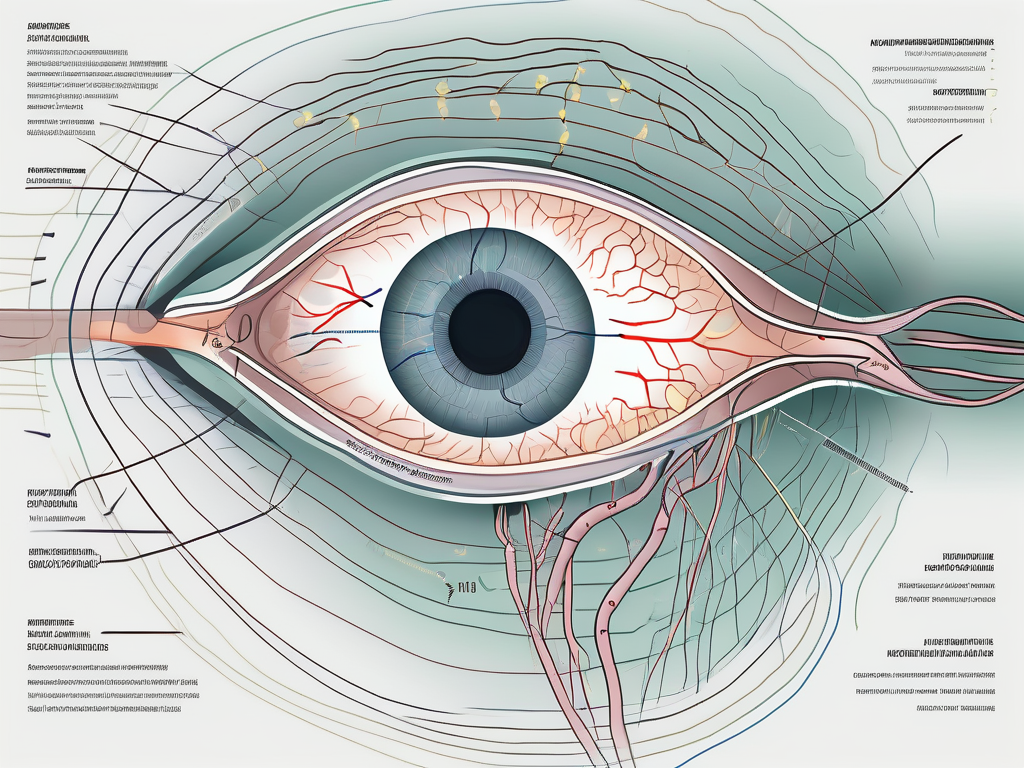
Anatomy of the Eye Relevant to Parasympathetic Control
The iris, a circular structure surrounding the pupil, has two types of smooth muscle: the sphincter pupillae and the dilator pupillae. The sphincter pupillae, controlled by the parasympathetic nervous system, causes pupillary constriction, while the dilator pupillae, controlled by the sympathetic nervous system, causes pupillary dilation.
The parasympathetic nerve fibers that control the sphincter pupillae are derived from the Edinger-Westphal nucleus and travel through the oculomotor nerve (CN III). These fibers synapse with the ciliary ganglion, located near the back of the eye.
The ciliary ganglion is a small cluster of nerve cell bodies that serves as a relay station for parasympathetic signals. It receives input from the Edinger-Westphal nucleus and sends out motor fibers to the sphincter pupillae muscle. This intricate network ensures precise control over pupillary constriction.
Interestingly, the parasympathetic nerve fibers that control the sphincter pupillae also play a role in regulating the shape of the lens. These fibers innervate the ciliary muscle, which is responsible for altering the shape of the lens to facilitate near vision. This process, known as accommodation, allows the eye to focus on objects at varying distances.
The Parasympathetic Nerve’s Role in Eye Function
The parasympathetic nerve’s role in eye function is not limited to pupillary constriction alone. It also regulates other aspects of eye functioning, such as accommodation and tear production.
Accommodation refers to the eye’s ability to change its focus from distant to near objects. The parasympathetic nervous system plays a vital role in this process by controlling the ciliary muscle, which alters the shape of the lens to facilitate near vision. This intricate coordination between the parasympathetic nervous system and the ciliary muscle allows for clear vision at various distances.
Tear production is also regulated by the parasympathetic nervous system. When activated, it stimulates the lacrimal glands to produce tears, keeping the eyes lubricated and protected. Tears not only provide moisture to the eyes but also contain essential enzymes and antibodies that help fight off infections and maintain ocular health.
In addition to pupillary constriction, accommodation, and tear production, the parasympathetic nerve also influences other aspects of eye function. It modulates the blood flow to the eye, ensuring an adequate supply of oxygen and nutrients to the various ocular structures. Furthermore, the parasympathetic nervous system coordinates with other cranial nerves to control eye movements, allowing for precise tracking of objects and maintaining visual stability.
In conclusion, the parasympathetic nerve plays a crucial role in the functioning of the eye. Its control over pupillary constriction, accommodation, tear production, blood flow regulation, and eye movements highlights its intricate involvement in maintaining optimal visual function and ocular health.
Pupillary Function and the Parasympathetic Nerve
Pupillary function is a dynamic process that serves different purposes, including regulating the amount of light entering the eye and maintaining optimal visual acuity. The parasympathetic nerve plays a significant role in pupillary function by controlling pupillary constriction and dilation.
The pupillary response is a fascinating mechanism that involves the coordination of various neural pathways. It is a finely tuned system that ensures our eyes adapt to changes in light levels and visual demands. Let’s delve deeper into the mechanism of pupillary constriction and dilation.
The Mechanism of Pupillary Constriction and Dilation
Pupillary constriction and dilation are regulated by a delicate balance between the parasympathetic and sympathetic nervous systems. When the parasympathetic nerve is activated, it releases acetylcholine, a neurotransmitter that binds to receptors in the sphincter pupillae muscle. This binding triggers a cascade of events that ultimately leads to the contraction of the muscle, resulting in pupillary constriction.
On the other hand, the sympathetic nervous system releases norepinephrine, which acts on receptors in the dilator pupillae muscle. This activation causes the muscle to contract, leading to pupillary dilation. The interplay between these two opposing forces ensures that our pupils respond appropriately to changes in light intensity and visual demands.
The regulation of pupillary function is not limited to the parasympathetic and sympathetic nervous systems alone. Various reflexes also contribute to the precise control of the pupillary response.
The Reflexes Involved in Pupillary Regulation
Two essential reflexes play a crucial role in pupillary regulation: the pupillary light reflex (PLR) and the near reflex.
The pupillary light reflex is a protective mechanism that adjusts the size of the pupils in response to changes in ambient light. When light enters the eye, it stimulates specialized cells called photoreceptors in the retina. These photoreceptors send signals to the brain, which then activates the parasympathetic pathway. The parasympathetic nerve releases acetylcholine, causing the sphincter pupillae to contract and resulting in pupillary constriction.
The near reflex, on the other hand, is responsible for adjusting the size of the pupils based on the visual demands of nearby objects. When we focus on a close object, a signal is sent from the brain to the ciliary muscles in the eye, causing them to contract. This contraction leads to accommodation, allowing us to see objects clearly at different distances. Simultaneously, the parasympathetic pathway is activated, resulting in pupillary constriction to enhance visual acuity.
The Parasympathetic Nerve’s Influence on Pupillary Function
Any dysfunction or disruption in the parasympathetic nerve’s control over pupillary function can lead to significant consequences. One such condition is Adie’s pupil, which occurs due to damage to the parasympathetic nerve fibers. Individuals with Adie’s pupil have a dilated pupil that reacts poorly to light but exhibits a stronger response to near stimuli. This condition can affect one or both eyes and often presents with additional symptoms such as decreased deep tendon reflexes.
Furthermore, disorders affecting the parasympathetic nervous system, such as diabetes or certain autoimmune conditions, can also result in pupillary dysfunction. In these cases, the parasympathetic nerve’s ability to control pupillary constriction and dilation may be impaired. This impairment can lead to abnormal pupil responses or fixed pupils, affecting the individual’s visual function and overall quality of life.
Understanding the intricate relationship between pupillary function and the parasympathetic nerve is essential in diagnosing and managing various eye conditions. Further research in this field will continue to shed light on the complex mechanisms that govern our pupillary response and its implications for human health.
Disorders Related to Parasympathetic Nerve Dysfunction in Pupillary Function
Several disorders can arise from parasympathetic nerve dysfunction, affecting pupillary function and overall eye health. It is important to recognize the symptoms associated with such disorders and seek appropriate medical attention for evaluation and treatment.
Parasympathetic nerve dysfunction in the eye can have a significant impact on an individual’s visual health. The parasympathetic nervous system is responsible for controlling the constriction of the pupil, which plays a crucial role in regulating the amount of light that enters the eye. When this system malfunctions, it can lead to a variety of symptoms and visual disturbances.
Symptoms of parasympathetic nerve dysfunction in the eye can vary depending on the specific condition and underlying cause. Common symptoms may include impaired pupillary constriction, abnormal pupil size, and altered responses to light and near stimuli. Moreover, individuals may experience accompanying vision problems, such as blurred vision or difficulty focusing.
If you experience any of these symptoms, it is important to consult with an eye care professional or a healthcare provider experienced in neuro-ophthalmology. They can assess your symptoms, conduct a comprehensive eye examination, and determine the underlying cause of the pupillary dysfunction.
Diagnosing the specific disorder related to parasympathetic nerve dysfunction requires a thorough evaluation of the patient’s medical history, a detailed examination of the eye, and potentially additional diagnostic tests. These tests may include pupillary reflex tests, imaging studies, or specialized electrophysiological tests to assess the function of the parasympathetic nervous system.
The treatment and management of parasympathetic nerve dysfunction in pupillary function depend on the underlying cause and severity of the condition. In some cases, addressing the primary cause, such as managing diabetes or treating an autoimmune disorder, may help alleviate pupillary dysfunction.
Additionally, individuals may benefit from certain medications or interventions that aim to compensate for the impaired parasympathetic control. These may include the use of miotic eye drops, which help constrict the pupil, or the use of contact lenses or glasses to improve visual acuity.
However, it is crucial to consult with a qualified healthcare professional before initiating any treatment, as they can provide a comprehensive evaluation and guide you towards appropriate interventions. They will consider factors such as the individual’s overall health, the severity of the pupillary dysfunction, and any potential risks or side effects associated with the proposed treatment options.
In conclusion, parasympathetic nerve dysfunction can have a significant impact on pupillary function and overall eye health. Recognizing the symptoms associated with these disorders and seeking appropriate medical attention is crucial for accurate diagnosis and effective management. With the guidance of a healthcare professional, individuals can explore various treatment options to alleviate pupillary dysfunction and improve their visual health.
Future Research Directions in Parasympathetic Nerve and Pupillary Function
Ongoing research is dedicated to further understanding the intricate relationship between the parasympathetic nerve and pupillary function. Studying the parasympathetic nervous system’s role in pupillary regulation can lead to advancements in diagnosing and managing various eye disorders.
Emerging Techniques in Studying Parasympathetic Nerve Function
Advancements in medical imaging techniques, such as functional magnetic resonance imaging (fMRI) and optical coherence tomography (OCT), have allowed researchers to investigate the parasympathetic nerve’s function in greater detail. By studying the neural pathways responsible for controlling pupillary function, researchers can gain insights into the underlying mechanisms and develop targeted interventions.
Functional magnetic resonance imaging (fMRI) is a non-invasive imaging technique that measures brain activity by detecting changes in blood flow. This technique has been used to study the parasympathetic nerve’s involvement in pupillary function. By observing changes in brain activity during pupillary constriction and dilation, researchers can map out the specific brain regions involved in regulating these processes.
Optical coherence tomography (OCT) is another imaging technique that provides high-resolution cross-sectional images of the eye. It has been used to visualize the structures of the eye, including the iris and ciliary body, which are involved in pupillary regulation. By analyzing these images, researchers can identify any structural abnormalities that may contribute to pupillary dysfunction.
Potential Therapeutic Advances for Pupillary Function Disorders
Understanding the role of the parasympathetic nerve in pupillary function opens doors for potential therapeutic advances. Researchers are exploring pharmacological agents that specifically target the parasympathetic pathway to improve pupillary regulation.
One potential therapeutic approach is the use of cholinergic agonists, which mimic the effects of acetylcholine, the neurotransmitter responsible for activating the parasympathetic nervous system. By administering these agents, researchers aim to enhance the parasympathetic activity and improve pupillary constriction.
In addition to pharmacological interventions, researchers are also investigating novel treatment modalities that can directly stimulate the parasympathetic nerve. Nerve stimulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and transcranial magnetic stimulation (TMS), have shown promise in modulating neural activity and may offer potential avenues for managing pupillary disorders in the future.
It is important to note that while these emerging techniques and potential therapeutic advances hold promise, further research is needed to fully understand their efficacy and safety in clinical settings. Collaborative efforts between researchers, clinicians, and industry partners are essential to translate these findings into practical applications that can benefit patients.
In conclusion, the parasympathetic nerve is a crucial component in the intricate process of pupillary function. Its role in regulating pupillary constriction, accommodation, and tear production highlights its significance in maintaining optimal eye health. Understanding the implications of the parasympathetic nerve’s dysfunction in pupillary function can lead to improved diagnosis, management, and potential therapeutic interventions for various eye disorders. If you experience any pupillary abnormalities or related symptoms, it is always advisable to consult with a healthcare professional with expertise in ophthalmology or neuro-ophthalmology for appropriate evaluation and guidance.