Femoral artery neuropathy can be a debilitating condition that affects many individuals. The discomfort and limitations it causes can significantly impact a person’s quality of life. However, there is hope on the horizon in the form of a promising treatment approach known as parasympathetic nerve block.
Understanding Femoral Artery Neuropathy
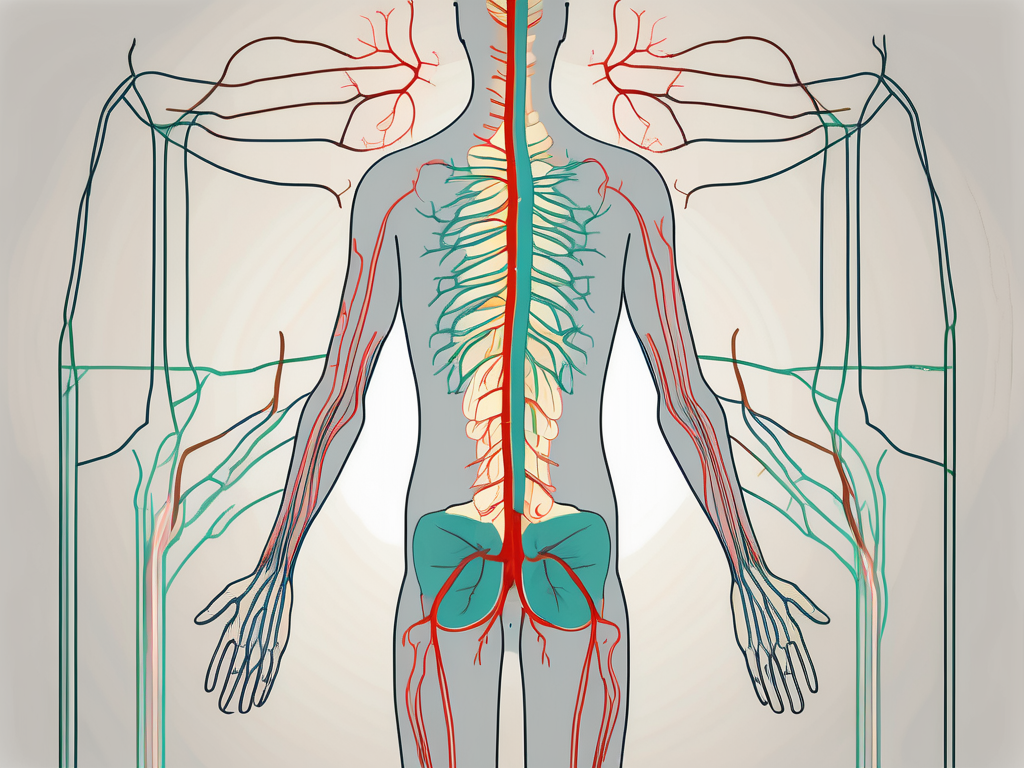
Before delving into the effectiveness of parasympathetic nerve block, it is essential to grasp the complexities surrounding femoral artery neuropathy. This condition arises when the femoral artery, located in the thigh, becomes compressed or damaged, leading to nerve dysfunction. Understanding the anatomy of the femoral artery is crucial in comprehending the mechanisms behind this neuropathy.
Femoral artery neuropathy is a condition that affects the femoral artery, one of the major blood vessels in the body. The femoral artery plays a vital role in supplying oxygenated blood to the lower limb. It runs down the front of the thigh, carrying essential nutrients to the muscles and tissues. However, when the femoral artery undergoes compression or damage, it can result in nerve irritation and pain.
The femoral artery is a complex structure, consisting of multiple layers and branches. It originates from the external iliac artery, which is located in the pelvis. As it travels down the thigh, it gives off various branches that supply blood to different areas, including the muscles and skin of the thigh.
The Anatomy of the Femoral Artery
The femoral artery is surrounded by various structures, including muscles, tendons, and nerves. These surrounding structures play a crucial role in maintaining the integrity and function of the artery. However, when there is compression or damage to these structures, it can lead to femoral artery neuropathy.
One of the main causes of femoral artery neuropathy is external compression. This can occur due to factors such as tight clothing, prolonged sitting or standing in a certain position, or trauma to the thigh. The compression can put pressure on the artery, leading to reduced blood flow and nerve dysfunction.
In addition to external compression, other factors can contribute to femoral artery neuropathy. These include atherosclerosis, which is the buildup of plaque in the artery walls, and vascular diseases such as diabetes or peripheral artery disease. These conditions can cause narrowing or blockage of the artery, resulting in reduced blood flow and nerve damage.
Symptoms and Diagnosis of Femoral Artery Neuropathy
Recognizing the symptoms of femoral artery neuropathy is crucial for early intervention and appropriate treatment. Common symptoms include thigh pain, numbness, tingling, and weakness in the affected leg. These symptoms can vary in severity and may worsen with activity or certain movements.
Diagnosis of femoral artery neuropathy usually involves a thorough medical examination, imaging tests, and evaluating the patient’s medical history. The healthcare provider will assess the patient’s symptoms, perform a physical examination of the affected leg, and may order imaging tests such as ultrasound or magnetic resonance imaging (MRI) to visualize the femoral artery and surrounding structures.
In some cases, additional tests may be necessary to determine the underlying cause of the neuropathy. This may include blood tests to check for conditions such as diabetes or atherosclerosis, or nerve conduction studies to assess the function of the nerves in the affected leg.
Current Treatment Options and Their Limitations
The current treatment options for femoral artery neuropathy focus primarily on pain management and addressing the underlying cause. Conservative approaches, such as physical therapy, pain medications, and lifestyle modifications, are commonly recommended to alleviate symptoms and improve overall leg function.
Physical therapy plays a crucial role in the management of femoral artery neuropathy. It aims to strengthen the muscles surrounding the femoral artery, improve flexibility, and promote proper blood flow. Pain medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, may be prescribed to manage pain and discomfort.
In cases where the underlying cause of the neuropathy is atherosclerosis or vascular disease, additional interventions may be necessary. These may include lifestyle modifications, such as adopting a healthy diet and regular exercise, or procedures to restore blood flow, such as angioplasty or bypass surgery.
However, it is important to note that these treatment options may only provide temporary relief or fail to address the root cause of the condition. As a result, some patients may seek more effective alternatives, such as parasympathetic nerve block, to alleviate their symptoms and improve their quality of life.
The Parasympathetic Nervous System and Its Role in Pain Management
Understanding the role of the parasympathetic nervous system in pain management is essential to appreciate the potential impact of parasympathetic nerve block as a treatment approach.
The Function of the Parasympathetic Nervous System
The parasympathetic nervous system is responsible for the body’s relaxation response, promoting rest, and digestion. It counterbalances the sympathetic nervous system, which is associated with the “fight or flight” response. By stimulating the parasympathetic nervous system, it is possible to lower pain perception and induce a state of calmness and relaxation.
When the parasympathetic nervous system is activated, it releases neurotransmitters such as acetylcholine, which bind to receptors in various organs and tissues throughout the body. These receptors initiate a cascade of physiological responses that promote relaxation and restoration.
One of the key ways in which the parasympathetic nervous system promotes relaxation is through its effect on the cardiovascular system. When activated, it causes blood vessels to dilate, reducing blood pressure and heart rate. This decrease in cardiovascular activity helps to create an overall sense of calmness and tranquility.
In addition to its cardiovascular effects, the parasympathetic nervous system also plays a crucial role in digestion. It stimulates the production of digestive enzymes and increases blood flow to the gastrointestinal tract, promoting efficient digestion and nutrient absorption. By optimizing the digestive process, the parasympathetic nervous system supports overall health and well-being.
Parasympathetic Nervous System’s Role in Neuropathic Pain
Neuropathic pain is often characterized by abnormal nerve signaling, resulting in chronic pain and discomfort. By targeting the parasympathetic nervous system, medical professionals have the potential to alleviate neuropathic pain by modulating the pain response and interrupting the pain signals being sent from the nerves.
One way in which the parasympathetic nervous system can help manage neuropathic pain is through the release of endogenous opioids. These naturally occurring substances bind to opioid receptors in the brain and spinal cord, inhibiting the transmission of pain signals. By activating the parasympathetic nervous system, the body can increase the production and release of endogenous opioids, providing pain relief.
Furthermore, the parasympathetic nervous system can also influence the release of other neurotransmitters involved in pain modulation, such as serotonin and norepinephrine. These neurotransmitters play a role in regulating mood, sleep, and pain perception. By enhancing the parasympathetic activity, it is possible to increase the availability of these neurotransmitters, leading to a reduction in neuropathic pain symptoms.
Additionally, the parasympathetic nervous system’s role in promoting relaxation and reducing stress can indirectly contribute to pain management. Chronic pain often leads to increased stress levels, which can exacerbate pain perception and create a vicious cycle. By activating the parasympathetic nervous system, individuals may experience a decrease in stress and anxiety, leading to a more positive pain management outcome.
In conclusion, the parasympathetic nervous system plays a crucial role in pain management, particularly in the context of neuropathic pain. By understanding its function and mechanisms of action, medical professionals can explore innovative treatment approaches, such as parasympathetic nerve block, to provide effective pain relief and improve the overall well-being of patients.
Parasympathetic Nerve Block: A New Hope for Patients
Parasympathetic nerve block is emerging as an innovative approach for the treatment of femoral artery neuropathy, offering hope for patients who have exhausted traditional treatment options.
Femoral artery neuropathy is a condition characterized by damage or dysfunction of the femoral nerve, which is responsible for transmitting sensory and motor signals to the lower extremities. This condition can cause debilitating pain, numbness, and weakness in the affected leg, significantly impacting a patient’s quality of life.
Traditional treatment options for femoral artery neuropathy often involve medication management, physical therapy, and in severe cases, surgical intervention. However, these approaches may not always provide adequate pain relief or address the underlying cause of the condition.
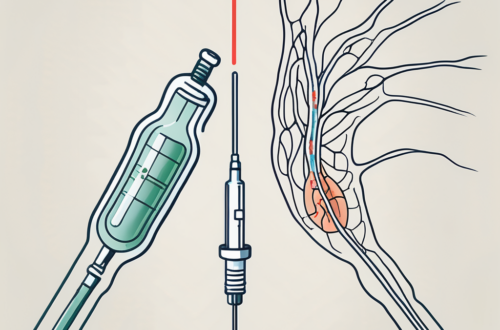
The Science Behind Parasympathetic Nerve Block
Parasympathetic nerve block involves injecting a local anesthetic near the femoral artery to block the transmission of pain signals. By specifically targeting the parasympathetic nerve fibers, this procedure aims to disrupt the abnormal pain signaling associated with femoral artery neuropathy.
The parasympathetic nervous system is responsible for regulating various bodily functions, including heart rate, digestion, and relaxation. By blocking the parasympathetic nerve fibers near the femoral artery, the pain signals originating from the damaged nerve can be effectively interrupted, providing relief to the patient.
The procedure is typically performed under the guidance of imaging techniques, such as ultrasound or fluoroscopy, to ensure accurate needle placement and minimize the risk of complications.
Potential Benefits of Parasympathetic Nerve Block for Femoral Artery Neuropathy
The potential benefits of parasympathetic nerve block are promising. By interrupting the pain signals associated with femoral artery neuropathy, patients may experience significant pain relief, improved mobility, and enhanced overall quality of life. The reduction in pain can also allow patients to engage in physical therapy more effectively, further aiding in their recovery.
Furthermore, parasympathetic nerve block is a minimally invasive procedure that can be performed on an outpatient basis, minimizing the need for hospitalization and reducing healthcare costs. This makes it a viable option for patients who may not be suitable candidates for more invasive surgical interventions.
However, it is important to note that individual responses to the procedure may vary. Some patients may experience complete pain relief, while others may only experience partial relief. The effectiveness of the parasympathetic nerve block may also depend on the severity and underlying cause of the femoral artery neuropathy.
Risks and Considerations in Parasympathetic Nerve Block Treatment
As with any medical procedure, parasympathetic nerve block does carry potential risks and considerations. These may include infection, bleeding, nerve damage, or an allergic reaction to the anesthetic used. It is crucial for patients to consult with a qualified healthcare professional to understand the potential risks and benefits specific to their condition.
Additionally, parasympathetic nerve block may not be suitable for all patients. Individuals with certain medical conditions, such as bleeding disorders or active infections, may not be eligible for the procedure. A thorough evaluation of the patient’s medical history and a comprehensive discussion with the healthcare provider are essential to determine the appropriateness of parasympathetic nerve block as a treatment option.
It is also important to note that parasympathetic nerve block is not a permanent solution for femoral artery neuropathy. The duration of pain relief varies among patients, and the procedure may need to be repeated periodically to maintain the desired effect.
In conclusion, parasympathetic nerve block offers a new hope for patients suffering from femoral artery neuropathy. With its potential to provide significant pain relief and improve overall quality of life, this innovative approach is paving the way for a more effective and minimally invasive treatment option. However, careful consideration of the potential risks and benefits, along with a thorough evaluation by a healthcare professional, is crucial in determining the suitability of parasympathetic nerve block for each individual patient.
Future Directions in Neuropathic Pain Management
The field of neuropathic pain management is constantly evolving, with ongoing research and advancements paving the way for more personalized and effective treatment approaches.
Neuropathic pain, characterized by abnormal pain signaling in the nervous system, can be a debilitating condition that significantly impacts a person’s quality of life. While current treatment options provide some relief, there is still a need for further advancements to optimize pain management strategies.
Advancements in Nerve Block Techniques
Ongoing advancements in nerve block techniques, such as parasympathetic nerve block, hold promise for the treatment of femoral artery neuropathy and other neuropathic conditions. These innovative techniques aim to provide targeted pain relief with minimal side effects, ultimately enhancing patient outcomes.
Parasympathetic nerve block involves the administration of local anesthetics or neurolytic agents to selectively block the parasympathetic nervous system, which plays a role in pain transmission and modulation. By interrupting abnormal pain signaling, this procedure offers hope for significant pain relief and improved quality of life for individuals suffering from femoral artery neuropathy.
The Potential of Personalized Pain Management
Personalized pain management approaches, guided by individual patient characteristics, are gaining recognition as a potential future direction in the field. By tailoring treatment plans according to a patient’s unique needs, healthcare professionals can optimize pain relief and improve overall treatment outcomes.
Advancements in technology, such as genetic testing and biomarker analysis, allow healthcare professionals to better understand the underlying mechanisms of neuropathic pain and identify specific factors that contribute to an individual’s pain experience. This personalized approach enables healthcare professionals to select the most appropriate treatment options, including medication choices, physical therapy techniques, and psychological interventions, based on the patient’s specific needs and preferences.
The Role of Research in Advancing Neuropathic Pain Treatments
Research plays a fundamental role in advancing the understanding and treatment of neuropathic pain. Ongoing studies exploring the mechanisms behind femoral artery neuropathy and the effectiveness of novel treatment approaches, such as parasympathetic nerve block, contribute to the development of evidence-based and transformative treatments in the field.
Researchers are investigating various aspects of neuropathic pain, including the role of inflammation, nerve regeneration, and central sensitization. By unraveling the complex mechanisms underlying neuropathic pain, scientists hope to identify new targets for intervention and develop innovative treatment strategies that can provide long-lasting relief.
Additionally, clinical trials are essential in evaluating the safety and efficacy of emerging treatments. These trials involve rigorous testing and monitoring to ensure that new interventions meet the highest standards of evidence-based medicine. Through collaborative efforts between researchers, healthcare professionals, and patients, the field of neuropathic pain management continues to advance, offering hope for improved outcomes and quality of life for individuals with femoral artery neuropathy.
In conclusion, parasympathetic nerve block holds promise as a treatment approach for individuals suffering from femoral artery neuropathy. By targeting the parasympathetic nervous system and interrupting abnormal pain signaling, this innovative procedure offers hope for significant pain relief and improved quality of life. However, it is important for patients to consult with their healthcare professionals to determine the best course of treatment for their specific condition.
As the field of neuropathic pain management continues to evolve, ongoing research and advancements pave the way for more personalized and effective treatment approaches, ultimately improving outcomes for individuals with femoral artery neuropathy. With a multidisciplinary approach and a commitment to scientific inquiry, healthcare professionals strive to alleviate the burden of neuropathic pain and enhance the well-being of those affected by this challenging condition.