Parasympathetic nerve impulses play a crucial role in regulating various bodily functions. Understanding how certain medications inhibit the transmission of these nerve impulses is essential for both medical professionals and patients alike. In this article, we will explore the intricate mechanism of nerve impulse transmission and delve into the specific medications that inhibit parasympathetic nerve impulses. Furthermore, we will discuss the therapeutic implications of utilizing these medications and highlight the potential future developments in this field.
Understanding Parasympathetic Nerve Impulses
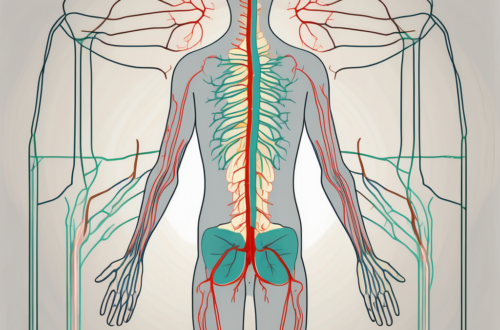
To comprehend the action of medications inhibiting parasympathetic nerve impulses, it is imperative to have a clear understanding of the role these nerves play in the body. The parasympathetic nervous system, alongside the sympathetic nervous system, constitutes the autonomic nervous system, which regulates involuntary bodily functions.
The parasympathetic nerves primarily control activities such as digestion, urination, and resting heart rate. They act in opposition to the sympathetic nerves, which are responsible for the fight-or-flight response.
The Role of Parasympathetic Nerves in the Body
Parasympathetic nerves emerge from specific areas of the spinal cord and cranial nerves. They innervate various organs, glands, and smooth muscles, ensuring the proper functioning of bodily systems. By stimulating these structures, parasympathetic nerves help maintain a state of rest and digestion, allowing the body to conserve energy.
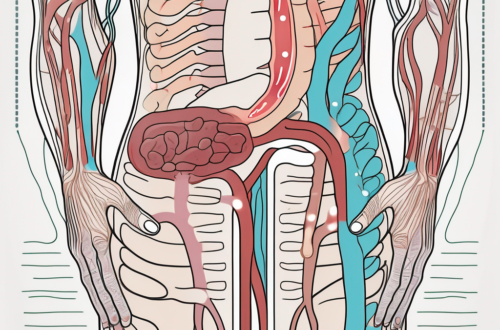
For example, when you sit down to enjoy a meal, your parasympathetic nerves kick in to stimulate the digestive system. They increase the secretion of digestive enzymes, enhance blood flow to the stomach and intestines, and promote the contraction of smooth muscles to facilitate the movement of food through the digestive tract. Without the parasympathetic nerves, the process of digestion would be compromised, leading to various gastrointestinal issues.
In addition to digestion, parasympathetic nerves also play a crucial role in regulating urination. When your bladder is full, these nerves send signals to the bladder muscles, causing them to contract and expel urine. Simultaneously, the parasympathetic nerves relax the muscles of the urinary sphincter, allowing the urine to flow out smoothly. Without the proper functioning of these nerves, urinary retention or incontinence can occur, leading to discomfort and potential urinary tract infections.
The Process of Nerve Impulse Transmission
Nerve impulse transmission involves a complex electrochemical mechanism. When a parasympathetic nerve is stimulated, it releases a neurotransmitter called acetylcholine. Acetylcholine then binds to specific receptors on the target cells, triggering a response. This response can either be excitatory, stimulating the target organ, or inhibitory, reducing its activity.
For instance, when you are in a state of deep relaxation, your parasympathetic nerves release acetylcholine, which binds to receptors on the heart muscle cells. This binding slows down the heart rate, allowing you to experience a calm and restful state. On the other hand, during moments of stress or danger, the sympathetic nerves release adrenaline, which overrides the effects of acetylcholine and increases the heart rate, preparing your body for action.
Understanding the process of nerve impulse transmission is crucial in comprehending the action of medications that inhibit parasympathetic nerve impulses. These medications work by blocking the receptors that acetylcholine binds to, thereby reducing the parasympathetic activity. This can be beneficial in certain medical conditions where excessive parasympathetic stimulation needs to be controlled, such as in the treatment of overactive bladder or certain gastrointestinal disorders.
The Mechanism of Medications on Nerve Impulses
Now that we have a fundamental understanding of parasympathetic nerve impulses, let us delve into how medications interact with these impulses. Medications that inhibit the transmission of parasympathetic nerve impulses act by interfering with the release or action of acetylcholine.
Acetylcholine is a neurotransmitter that plays a crucial role in the parasympathetic nervous system. It is responsible for transmitting signals between nerve cells, allowing for the regulation of various bodily functions such as digestion, heart rate, and bladder control.
One common way medications inhibit parasympathetic nerve impulses is by blocking the receptors to which acetylcholine binds. By doing so, these medications prevent the normal physiological response triggered by acetylcholine, effectively reducing parasympathetic activity.
Imagine these receptors as tiny locks on the surface of the cells. When acetylcholine, the key, binds to these receptors, it unlocks a cascade of events that ultimately leads to the desired bodily response. However, medications can act as master keys, fitting into these receptors and preventing acetylcholine from binding. This interruption in the signaling process dampens the parasympathetic response, bringing relief to certain medical conditions.
Other medications may work by affecting the release of acetylcholine or interfering with the synthesis of this neurotransmitter. These complex mechanisms allow for targeted control and modulation of parasympathetic nerve impulses.
For instance, some medications can inhibit the enzyme responsible for breaking down acetylcholine, leading to an increase in its availability and prolonged effects. This can be beneficial in managing conditions where enhanced parasympathetic activity is desired, such as certain types of glaucoma.
The Impact of Medications on Parasympathetic Nerve Function
The use of medications that inhibit parasympathetic nerve impulses can have a profound impact on a range of medical conditions. Such medications may be prescribed to manage conditions such as overactive bladder, gastrointestinal disorders, or even certain cardiovascular conditions.
Overactive bladder, for example, is a condition characterized by an uncontrollable urge to urinate. Medications that inhibit parasympathetic nerve impulses can help relax the bladder muscles, reducing the frequency and urgency of urination.
Gastrointestinal disorders, such as irritable bowel syndrome, can also benefit from medications that target parasympathetic nerve impulses. By modulating the activity of the parasympathetic nervous system in the digestive tract, these medications can help alleviate symptoms like abdominal pain, bloating, and irregular bowel movements.
In certain cardiovascular conditions, medications that inhibit parasympathetic nerve impulses can be used to manage heart rate and blood pressure. By reducing the parasympathetic activity that slows down the heart rate, these medications can help regulate heart rhythm and improve blood flow.
It is important to note that the decision to utilize medication for inhibiting parasympathetic nerve impulses should always be made in consultation with a healthcare professional. Each patient’s unique medical history and symptoms must be carefully considered to ensure optimal treatment outcomes.
Furthermore, medications that affect parasympathetic nerve impulses may have side effects. These can include dry mouth, constipation, blurred vision, or even changes in heart rate. Close monitoring and regular follow-ups with a healthcare provider are essential to manage any potential risks and adjust the treatment plan as needed.
In conclusion, medications that interact with parasympathetic nerve impulses play a crucial role in managing various medical conditions. By understanding the mechanisms behind these medications, healthcare professionals can tailor treatment plans to optimize patient outcomes and improve their quality of life.
Specific Medications that Inhibit Parasympathetic Nerve Impulses
The inhibition of parasympathetic nerve impulses is a crucial aspect of medical treatment for various conditions. A variety of medications are classified as inhibitors of parasympathetic nerve impulses, each with their own unique mechanisms of action. These medications can be further classified based on their specific mechanisms of action, providing healthcare professionals with a range of options to choose from when prescribing treatment.
Classification of Inhibitory Medications
When it comes to inhibiting parasympathetic nerve impulses, healthcare professionals have several classes of medications at their disposal. These medications can be broadly classified into anticholinergic drugs, muscarinic receptor antagonists, and cholinesterase inhibitors. Each class of medications functions uniquely in inhibiting parasympathetic nerve impulses, providing healthcare professionals with a diverse range of treatment options.
The Action of Each Medication
Anticholinergic drugs, one of the classes of medications used to inhibit parasympathetic nerve impulses, work by blocking the receptors that acetylcholine would normally bind to. By doing so, these medications prevent the transmission of nerve impulses, effectively inhibiting the parasympathetic nervous system. This inhibition can be beneficial in certain medical conditions where reducing parasympathetic activity is desired.
Muscarinic receptor antagonists, another class of medications that inhibit parasympathetic nerve impulses, target specific subtypes of the receptors that respond to acetylcholine. By antagonizing these receptors, these medications effectively block the action of acetylcholine, leading to the inhibition of parasympathetic nerve impulses. This targeted approach allows healthcare professionals to selectively inhibit parasympathetic activity in specific areas of the body, providing precise control over the physiological response.
Cholinesterase inhibitors, on the other hand, take a different approach in inhibiting parasympathetic nerve impulses. Instead of blocking receptors or neurotransmitters, these medications work by increasing the availability of acetylcholine. By inhibiting the enzyme cholinesterase, which breaks down acetylcholine, these medications effectively enhance the levels of acetylcholine in the body. This increased availability of acetylcholine leads to enhanced parasympathetic nerve inhibition, providing relief in certain medical conditions where reducing parasympathetic activity is beneficial.
Understanding the mechanisms of action of these medications is essential for healthcare professionals when prescribing treatment. By selecting the appropriate class of medication based on the patient’s condition and desired therapeutic outcome, healthcare professionals can effectively inhibit parasympathetic nerve impulses and provide relief to patients suffering from various medical conditions.
The Therapeutic Implications of Inhibiting Parasympathetic Nerve Impulses
The parasympathetic nervous system plays a crucial role in regulating various bodily functions, including digestion, urination, and rest. However, in certain medical conditions, such as overactive bladder and gastrointestinal disorders characterized by hypermotility, inhibiting parasympathetic nerve impulses can offer significant therapeutic benefits.
Potential Benefits of Inhibitory Medications
One of the primary therapeutic benefits of inhibitory medications is their ability to reduce urinary urgency and frequency in individuals with overactive bladder. This can greatly improve the quality of life for those who experience frequent and uncontrollable urges to urinate.
In gastrointestinal disorders characterized by hypermotility, inhibitory medications can help alleviate symptoms such as abdominal pain, cramping, and diarrhea. By slowing down the excessive contractions of the intestines, these medications promote normal bowel function and provide relief to individuals suffering from these conditions.
Furthermore, inhibitory medications can also be used in the management of certain eye conditions. By blocking parasympathetic nerve impulses, these medications can help dilate the pupils, making it easier for eye care professionals to examine the retina and diagnose any potential abnormalities.
Possible Side Effects and Risks
While inhibitory medications can provide significant therapeutic relief, it is important to be aware of their potential side effects and risks. Common side effects may include dry mouth, blurred vision, constipation, or even cognitive impairments. These side effects are generally mild and temporary, but it is essential for patients to be aware of them and to discuss any concerns with their healthcare provider.
Additionally, certain populations, such as the elderly or individuals with specific medical conditions, may be more susceptible to adverse reactions from inhibitory medications. It is crucial to consult with a healthcare professional before initiating any medication regimen to ensure the appropriateness and safety of treatment.
Furthermore, it is important to note that inhibitory medications should be used under the guidance of a healthcare professional and in accordance with the prescribed dosage. Misuse or overuse of these medications can lead to complications and may not provide the desired therapeutic effects.
In conclusion, inhibiting parasympathetic nerve impulses through the use of medications can offer various therapeutic benefits in conditions such as overactive bladder, gastrointestinal disorders, and certain eye conditions. However, it is essential to be aware of the potential side effects and risks associated with these medications and to consult with a healthcare professional for personalized guidance and monitoring throughout the treatment process.
Future Directions in Medication Development
The Need for More Effective Inhibitory Medications
While current inhibitory medications can provide relief for many patients, there is a continuous need for more effective treatments. Ongoing research aims to develop medications with enhanced specificity and fewer side effects. Additionally, the exploration of novel targets and mechanisms of action holds promising potential in improving treatment outcomes.
One area of focus in medication development is the enhancement of specificity. Current inhibitory medications may have some degree of off-target effects, leading to unwanted side effects. Researchers are working to identify specific molecular targets that are responsible for nerve impulse inhibition, allowing for the development of medications that can selectively target these sites without affecting other physiological processes. By achieving greater specificity, the efficacy of inhibitory medications can be improved while minimizing side effects.
Another aspect being explored in medication development is the identification of novel targets and mechanisms of action. While current inhibitory medications primarily target well-known pathways involved in nerve impulse transmission, there may be undiscovered targets and mechanisms that can be harnessed for more effective inhibition. By expanding the understanding of the complex network of signaling molecules and receptors involved in nerve impulse transmission, researchers hope to uncover new therapeutic targets that can be exploited for the development of innovative inhibitory medications.
The Potential of Personalized Medicine in Nerve Impulse Inhibition
The field of personalized medicine offers exciting prospects in nerve impulse inhibition. By considering individual variations in genetic makeup, metabolism, and response to medications, tailored treatment plans can be designed. These personalized approaches have the potential to optimize therapeutic outcomes and minimize adverse effects.
Advancements in genetic research have revealed that variations in genes can influence an individual’s response to medications. By identifying specific genetic markers associated with the efficacy or adverse effects of inhibitory medications, healthcare providers can determine the most suitable treatment options for each patient. This approach, known as pharmacogenomics, allows for personalized medicine that takes into account an individual’s unique genetic profile, ensuring that the chosen inhibitory medication is most likely to be effective and well-tolerated.
In addition to genetic factors, personalized medicine in nerve impulse inhibition also considers an individual’s metabolism. Variations in drug metabolism enzymes can affect the rate at which medications are broken down and eliminated from the body. By assessing an individual’s metabolic profile, healthcare providers can adjust the dosage or choose alternative medications to ensure optimal inhibition of nerve impulses.
Furthermore, personalized medicine takes into account an individual’s response to medications. Some patients may experience greater therapeutic benefits from certain inhibitory medications, while others may have a limited response. By closely monitoring a patient’s response to treatment, healthcare providers can make necessary adjustments to the medication regimen, ensuring that the inhibitory effect on parasympathetic nerve impulses is maximized.
In conclusion, understanding the action of medications inhibiting the transmission of parasympathetic nerve impulses is crucial in the field of medicine. By exploring the intricate mechanism of nerve impulse transmission and gaining knowledge about inhibitory medications, medical professionals and patients can make informed decisions regarding treatment options. While medications offer therapeutic benefits, it is essential to consult with a healthcare provider to discuss individual circumstances and potential risks. The future of medication development holds promise in the quest for more effective and personalized treatments for inhibiting parasympathetic nerve impulses.