The parasympathetic nervous system plays a crucial role in regulating various physiological processes in the body, including heart rate. Understanding the intricate connection between the parasympathetic nerve and heart rate is essential for comprehending the physiological mechanisms behind heart rate regulation and its clinical implications.
Understanding the Parasympathetic Nervous System
The parasympathetic nervous system is one of the two divisions of the autonomic nervous system, alongside the sympathetic nervous system. While the sympathetic nervous system prepares the body for fight-or-flight responses, the parasympathetic nervous system promotes rest and relaxation.
When activated, the parasympathetic nervous system helps to conserve energy and maintain homeostasis by slowing down heart rate, among other functions. This system is primarily responsible for modulating heart rate during periods of rest and in response to certain stimuli.
But what exactly happens in the body when the parasympathetic nervous system is activated? Let’s delve deeper into its role and functions.
The Role of the Parasympathetic Nervous System in the Body
Beyond its influence on heart rate, the parasympathetic nervous system impacts several other bodily functions. It regulates digestion, controls the release of certain hormones, and aids in the mobilization of the body’s energy resources.
When the parasympathetic nervous system is activated, it produces a calming effect on the body. Blood pressure decreases, pupils constrict, and digestion is promoted. These responses work together to create an environment of rest and relaxation, allowing the body to recover and recharge.
Moreover, the parasympathetic nervous system plays a crucial role in maintaining overall physiological balance. It helps regulate the secretion of digestive enzymes, ensuring efficient breakdown and absorption of nutrients. Additionally, it stimulates the release of saliva, which aids in the initial stages of digestion.
Furthermore, this system influences the release of hormones such as insulin, which is responsible for regulating blood sugar levels. By promoting the release of insulin, the parasympathetic nervous system helps to maintain stable glucose levels in the body.
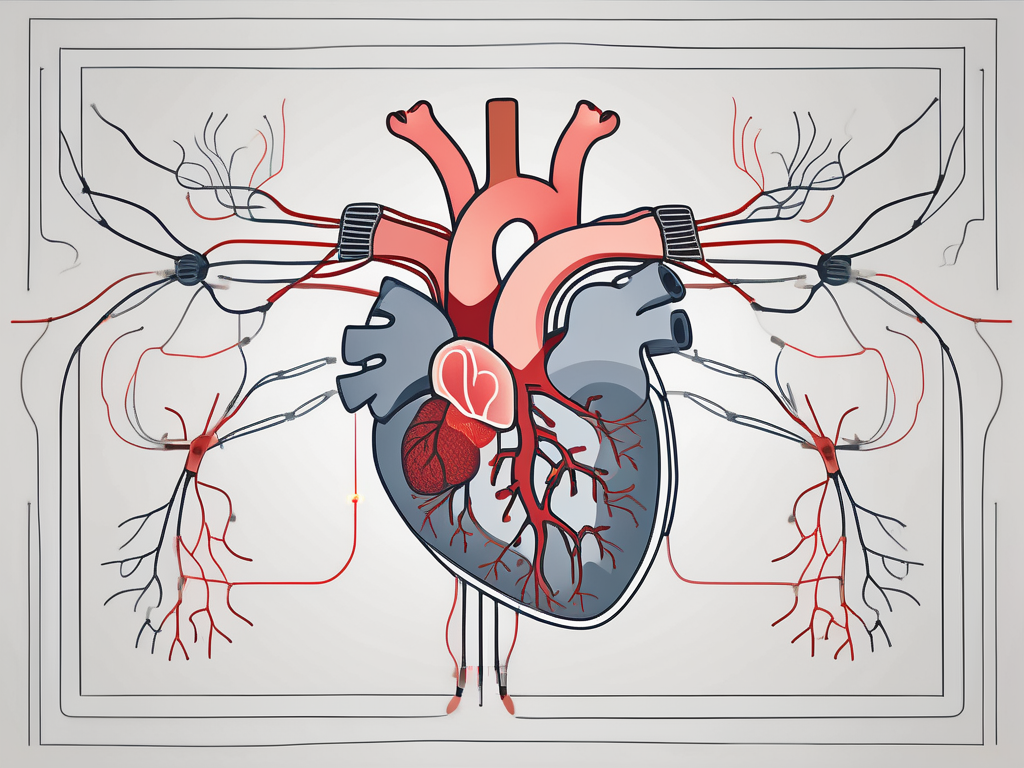
The Anatomy of the Parasympathetic Nervous System
The parasympathetic nervous system originates in the brainstem and extends through various cranial nerves and the spinal cord to innervate target organs. It primarily uses acetylcholine as its neurotransmitter to convey messages from nerve to nerve and nerve to muscle.
One of the key components of the parasympathetic nervous system is the vagus nerve. Emerging from the medulla oblongata, the vagus nerve innervates organs in the thoracic and abdominal cavities. It plays a vital role in regulating heart rate, controlling digestion, and influencing various other functions.
In addition to the vagus nerve, the parasympathetic innervation of pelvic organs is facilitated by the pelvic splanchnic nerves. These nerves contribute to the regulation of urinary and reproductive functions, ensuring proper bladder control, and facilitating sexual arousal and orgasm.
Overall, the parasympathetic nervous system is a complex network of nerves that work together to promote rest, relaxation, and the maintenance of physiological balance. Its intricate anatomy and functions highlight its importance in the overall functioning of the human body.
The Parasympathetic Nerve and Heart Rate Connection
Heart rate regulation involves a delicate balance between sympathetic and parasympathetic influences. The parasympathetic nerve, specifically the vagus nerve, plays a crucial role in slowing down heart rate and maintaining optimal cardiac function.
How the Parasympathetic Nerve Controls Heart Rate
When the body is at rest, the parasympathetic nervous system predominates, causing the vagus nerve to release acetylcholine onto the sinoatrial (SA) node of the heart. This inhibitory neurotransmitter binds to specific receptors, which slows down the firing rate of the SA node.
By reducing the rate at which electrical impulses travel through the heart, the parasympathetic nerve helps maintain a slower heart rate during periods of relaxation and non-strenuous activity.
However, the influence of the parasympathetic nerve on heart rate goes beyond simple neural control. It involves a complex interplay of biochemical processes that ensure the fine-tuning of heart rate in response to physiological demands.
The Biochemical Process Behind Heart Rate Regulation
Heart rate regulation involves complex biochemical processes that go beyond neural control. Factors such as circulating hormones, electrolyte balance, and metabolic state can influence heart rate.
For instance, the parasympathetic nervous system indirectly influences heart rate through biochemical pathways involving the release of hormones like acetylcholine, which affects the SA node’s electrical activity. These intricate biochemical interactions ensure the fine-tuning of heart rate in response to physiological demands.
In addition to hormonal influences, electrolyte balance also plays a significant role in heart rate regulation. Electrolytes, such as potassium and calcium, are essential for the proper functioning of cardiac cells. Imbalances in these electrolytes can disrupt the electrical signals within the heart, leading to abnormal heart rhythms and fluctuations in heart rate.
Furthermore, the metabolic state of the body can impact heart rate. During physical exercise or periods of increased metabolic demand, the body requires more oxygen and nutrients. In response, the sympathetic nervous system becomes more active, releasing hormones like adrenaline that increase heart rate and cardiac output to meet the heightened demand.
Conversely, during periods of rest and relaxation, the parasympathetic nervous system takes over, slowing down heart rate to conserve energy and promote recovery. This balance between sympathetic and parasympathetic influences ensures that the heart can adapt to varying physiological needs.
Overall, the regulation of heart rate is a complex process that involves the interplay of neural, hormonal, electrolyte, and metabolic factors. The parasympathetic nerve, with its release of acetylcholine onto the SA node, plays a crucial role in maintaining a slower heart rate during periods of rest and relaxation. Understanding these intricate mechanisms is essential for comprehending the delicate balance required for optimal cardiac function.
The Impact of Parasympathetic Nerve Stimulation on Heart Rate
Understanding the impact of parasympathetic nerve stimulation on heart rate variability and cardiac function is essential for assessing clinical implications and potential therapeutic interventions.
Parasympathetic nerve stimulation plays a crucial role in regulating heart rate and maintaining cardiovascular health. By exploring the effects of parasympathetic nerve stimulation on heart rate variability and cardiac function, researchers and healthcare professionals can gain valuable insights into autonomic function and cardiovascular well-being.
The Effect of Parasympathetic Nerve Stimulation on Heart Rate Variability
Heart rate variability refers to the beat-to-beat variation in the intervals between consecutive heartbeats. It serves as a valuable indicator of autonomic nervous system activity, with parasympathetic dominance associated with increased heart rate variability.
Parasympathetic nerve stimulation can lead to an augmented parasympathetic response, resulting in increased heart rate variability. This increase in variability is indicative of a healthy autonomic nervous system and reflects the ability of the heart to adapt to changing physiological demands.
Monitoring heart rate variability can provide insights into autonomic function, cardiovascular health, and response to therapy. By analyzing the patterns and fluctuations in heart rate variability, healthcare professionals can assess the overall health of the autonomic nervous system and identify potential abnormalities or dysfunctions.
The Influence of Parasympathetic Nerve Stimulation on Cardiac Function
Parasympathetic nerve stimulation can have both positive and negative effects on cardiac function. While parasympathetic dominance generally leads to lower heart rate and increased efficiency, excessive stimulation can result in bradycardia, decreased cardiac output, and compromised cardiovascular performance.
Understanding the optimal level and duration of parasympathetic nerve stimulation is crucial for maintaining cardiac function and avoiding potential complications. Healthcare professionals carefully evaluate the balance between sympathetic and parasympathetic activity to ensure the heart functions optimally and efficiently.
It is important to note that any therapeutic interventions involving parasympathetic nerve stimulation should be performed under the guidance of a healthcare professional. The expertise and knowledge of these professionals are essential in determining the appropriate course of action and minimizing the risks associated with parasympathetic nerve stimulation.
By continuously advancing our understanding of the impact of parasympathetic nerve stimulation on heart rate and cardiac function, researchers and healthcare professionals can develop targeted therapeutic interventions to address various cardiovascular conditions. This ongoing research and exploration hold great promise for improving patient outcomes and enhancing overall cardiovascular health.
The Clinical Implications of Parasympathetic Nerve Activity on Heart Rate
Altered parasympathetic nerve activity and impaired heart rate regulation can have significant clinical implications, particularly in the context of cardiovascular disease.
Parasympathetic nerve activity plays a crucial role in maintaining the balance of the autonomic nervous system, which regulates various bodily functions, including heart rate. When there is an imbalance in parasympathetic nerve activity, it can lead to dysregulation of heart rate, potentially resulting in adverse clinical outcomes.
Cardiovascular conditions such as heart failure, arrhythmias, and autonomic dysfunction often involve abnormal parasympathetic nerve activity. These dysfunctions can lead to abnormal heart rate patterns, compromised cardiac function, and increased morbidity and mortality.
For instance, in heart failure, there is a decrease in parasympathetic nerve activity and an increase in sympathetic nerve activity, resulting in an imbalance that leads to elevated heart rates and reduced cardiac output. This imbalance can further exacerbate the symptoms of heart failure and contribute to disease progression.
Similarly, in arrhythmias, abnormal parasympathetic nerve activity can disrupt the normal electrical conduction system of the heart, leading to irregular heart rhythms. These irregular rhythms can have serious clinical implications, including an increased risk of stroke, heart attack, and sudden cardiac death.
Moreover, autonomic dysfunction, which involves impaired regulation of the autonomic nervous system, can also affect parasympathetic nerve activity. This dysfunction can result from various underlying conditions, such as diabetes, Parkinson’s disease, and multiple system atrophy. In these cases, the altered parasympathetic nerve activity can contribute to cardiovascular complications, including orthostatic hypotension and abnormal heart rate responses to physical activity.
A thorough understanding of the interplay between parasympathetic nerve activity and cardiovascular disease can guide the development of targeted therapies and personalized treatment approaches. Researchers and clinicians are actively investigating novel interventions to modulate parasympathetic nerve activity and restore the autonomic balance in cardiovascular disease.
Therapeutic Potential of Parasympathetic Nerve Stimulation
Parasympathetic nerve stimulation techniques, such as vagus nerve stimulation, have shown promise in the management of various cardiac conditions. These therapies aim to enhance parasympathetic dominance and modulate heart rate to improve symptoms and overall cardiac function.
Vagus nerve stimulation involves the electrical stimulation of the vagus nerve, which is a major component of the parasympathetic nervous system. By activating the vagus nerve, the therapy promotes the release of acetylcholine, a neurotransmitter that slows down the heart rate and reduces cardiac contractility.
Studies have demonstrated the effectiveness of vagus nerve stimulation in conditions such as heart failure, atrial fibrillation, and ventricular tachycardia. The therapy has been shown to improve symptoms, reduce hospitalizations, and enhance quality of life for patients with these cardiac conditions.
While the therapeutic potential of parasympathetic nerve stimulation is an exciting frontier in medical research, it is imperative to emphasize that such interventions should be evaluated and administered by qualified medical professionals. The safety and efficacy of these therapies depend on proper patient selection, accurate device placement, and appropriate stimulation parameters.
Furthermore, ongoing research is exploring other approaches to modulate parasympathetic nerve activity, including pharmacological interventions and non-invasive neuromodulation techniques. These advancements hold promise for expanding the therapeutic options available for patients with cardiovascular disease.
Future Research Directions in Parasympathetic Nerve and Heart Rate Studies
Continued research in the field of parasympathetic nerve and heart rate regulation will undoubtedly shed light on novel mechanisms, therapeutic strategies, and diagnostic tools. This will lead to significant advancements in our understanding of cardiovascular health and the development of more effective treatments.
One promising area of future research is the exploration of the role of parasympathetic nerve activity in different physiological and pathological conditions. By studying the variations in parasympathetic nerve function across populations, researchers can identify potential risk factors for cardiovascular diseases and develop targeted interventions.
Furthermore, advancements in imaging techniques have the potential to revolutionize our understanding of parasympathetic nerve regulation. High-resolution imaging methods, such as magnetic resonance imaging (MRI) and positron emission tomography (PET), can provide detailed insights into the anatomical connections and functional interactions of the parasympathetic nervous system.
Challenges and Opportunities in Parasympathetic Nerve Research
Studying parasympathetic nerve activity presents unique challenges due to its intricate anatomical connections and complex physiological interactions. However, advances in imaging techniques, genetic studies, and computational modeling provide opportunities to overcome these challenges and deepen our understanding of this vital regulatory system.
Genetic studies, for instance, can help identify specific genes and genetic variants that influence parasympathetic nerve function. By understanding the genetic basis of parasympathetic nerve regulation, researchers can develop targeted therapies and interventions that can modulate the activity of this system.
Computational modeling is another powerful tool that can aid in unraveling the complexities of parasympathetic nerve regulation. By creating sophisticated mathematical models that simulate the interactions between different components of the parasympathetic nervous system, researchers can gain insights into the underlying mechanisms and predict the effects of interventions.
The Future of Heart Rate Management: A Look Ahead
The future of heart rate management lies in harnessing the power of personalized medicine, novel non-invasive therapies, and advanced technologies. With the advent of wearable devices and mobile health applications, individuals can now monitor their heart rate in real-time and make informed decisions about their cardiovascular health.
Personalized medicine, on the other hand, aims to tailor treatments and interventions to an individual’s unique characteristics, including their parasympathetic nerve activity. By considering factors such as genetics, lifestyle, and environmental influences, healthcare professionals can develop personalized treatment plans that optimize heart rate regulation and improve overall cardiovascular health.
Novel non-invasive therapies, such as transcutaneous vagus nerve stimulation, show promise in modulating parasympathetic nerve activity and regulating heart rate. This approach involves the application of electrical stimulation to the skin overlying the vagus nerve, which can enhance parasympathetic activity and promote cardiovascular health.
By unraveling the molecular, cellular, and systemic intricacies of parasympathetic nerve regulation of heart rate, researchers can enhance our ability to diagnose, treat, and prevent cardiovascular diseases effectively. This knowledge can inform the development of targeted therapies that specifically address the underlying causes of heart rate dysregulation.
In conclusion, understanding the profound impact of the parasympathetic nerve on heart rate regulation requires a comprehensive analysis of the intricate physiological mechanisms, clinical implications, and future research directions. As with any medical topic, it is essential to consult with a healthcare professional for personalized advice and appropriate management strategies. The ongoing research in this field holds great promise for improving cardiovascular health and enhancing the quality of life for individuals worldwide.