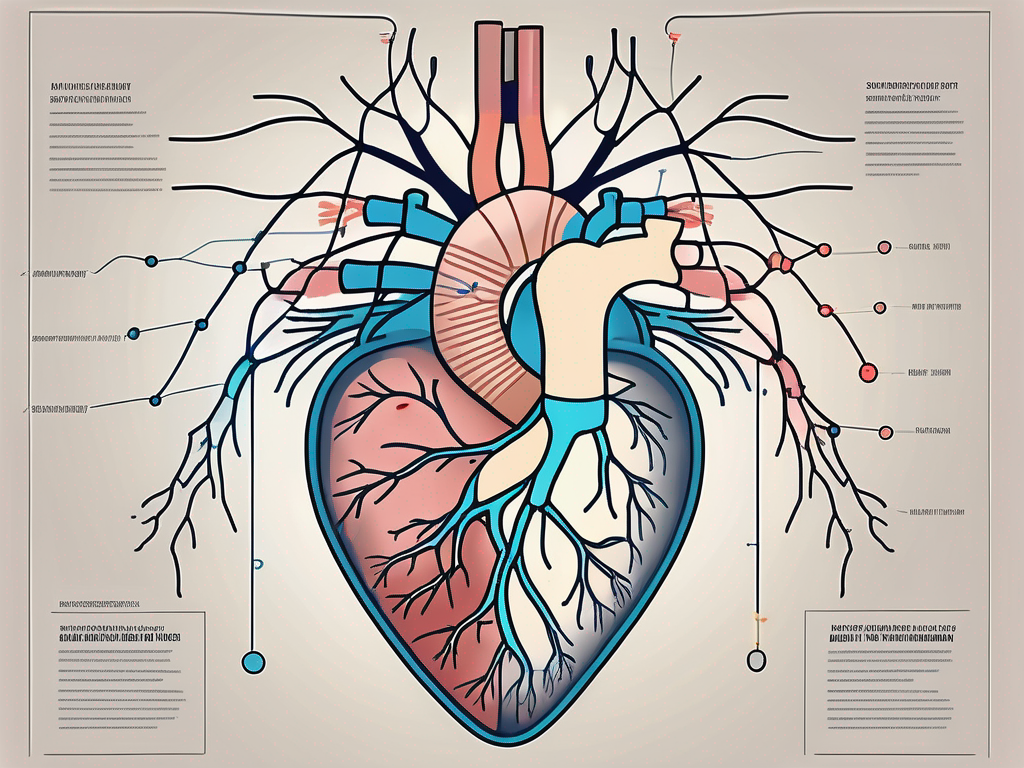
The heart is a vital organ responsible for pumping blood throughout the body, supplying oxygen and nutrients to all cells and tissues. The heart rate, the number of times the heart beats per minute, is crucial for maintaining optimal cardiovascular health. The regulation of heart rate is complex and involves the intricate interplay between the sympathetic and parasympathetic branches of the autonomic nervous system.
Understanding the Autonomic Nervous System
The autonomic nervous system (ANS) is an involuntary division of the peripheral nervous system that controls essential bodily functions. It consists of two main branches, namely the sympathetic and parasympathetic nervous systems. The sympathetic division is responsible for the “fight-or-flight” response, while the parasympathetic division promotes the body’s “rest-and-digest” activities.
The autonomic nervous system is a complex network of nerves that regulates various bodily functions without conscious effort. It controls processes such as heart rate, blood pressure, digestion, respiration, and body temperature. These functions are vital for the body to maintain homeostasis and respond to external stimuli.
Role of the Autonomic Nervous System in Heart Function
The ANS plays a crucial role in regulating heart function. It controls the rate and force of heart contractions, ensuring adequate blood supply to meet the body’s demands. The balance between sympathetic and parasympathetic activity is key in maintaining optimal heart rate.
When the body encounters a stressful situation or requires increased physical exertion, the sympathetic division of the autonomic nervous system is activated. This leads to the release of norepinephrine, a neurotransmitter that binds to receptors in the heart, causing an increase in heart rate and cardiac output. This physiological response prepares the body for action, enabling it to respond effectively to the perceived threat or demand.
On the other hand, during periods of rest and relaxation, the parasympathetic division of the autonomic nervous system takes over. It releases acetylcholine, another neurotransmitter that acts on the heart to decrease heart rate. This promotes a state of calmness and allows the body to conserve energy and recover from previous activities.
Sympathetic and Parasympathetic Nerves: An Overview
The sympathetic and parasympathetic branches of the ANS exert opposing effects on heart rate. The sympathetic nerves release norepinephrine, which increases heart rate and cardiac output, preparing the body for physical exertion or stress. On the other hand, the parasympathetic nerves release acetylcholine, which decreases heart rate, promoting relaxation and recovery.
In addition to their role in heart function, the sympathetic and parasympathetic divisions of the autonomic nervous system have distinct effects on other organs and systems in the body. The sympathetic division is responsible for dilating the pupils, increasing blood flow to skeletal muscles, and inhibiting digestive processes. It also triggers the release of stress hormones, such as adrenaline, which further enhance the body’s response to stress.
On the contrary, the parasympathetic division is responsible for constricting the pupils, promoting digestion and nutrient absorption, and reducing heart rate. It helps the body conserve energy and promotes restorative processes, such as tissue repair and growth.
Overall, the autonomic nervous system is a remarkable and intricate system that ensures the body functions optimally in various situations. Its ability to regulate heart rate, blood pressure, and other vital functions is essential for maintaining overall health and well-being.
The Sympathetic Nervous System and Heart Rate
The sympathetic nervous system plays a crucial role in regulating heart rate in response to stress, exercise, or other physiological demands. Activation of the sympathetic nerves increases heart rate, enhances cardiac contractility, and dilates blood vessels, redirecting blood flow to the muscles and the brain.
When the body encounters a stressful situation, such as a sudden loud noise or a perceived threat, the sympathetic nervous system springs into action. It releases a neurotransmitter called norepinephrine, which binds to beta-adrenergic receptors in the heart. This binding activates a cascade of intracellular events, leading to an increase in the firing rate of the heart’s pacemaker cells and promoting a faster heart rate.
Furthermore, sympathetic stimulation triggers the release of stress hormones, such as adrenaline, from the adrenal glands. These hormones further enhance heart rate and prepare the body for a “fight or flight” response. The increased heart rate ensures that oxygen and nutrients are delivered to the muscles and the brain, enabling the body to respond quickly and effectively to the perceived threat.
How the Sympathetic Nervous System Regulates Heart Rate
The sympathetic nervous system’s control over heart rate is a complex and finely tuned process. In addition to the release of norepinephrine and stress hormones, other factors come into play. For example, the sympathetic nerves also innervate the heart’s conduction system, which coordinates the electrical signals that regulate heart rhythm. By modulating the activity of these specialized cells, the sympathetic nervous system can further influence heart rate.
Moreover, the sympathetic nervous system’s impact on heart rate is not limited to acute stress situations. It also plays a role in regulating heart rate during exercise. As physical activity increases, the sympathetic nervous system is activated to meet the increased demand for oxygen and energy. This results in a gradual increase in heart rate, allowing the body to deliver more blood and nutrients to the working muscles.
The Impact of Stress on the Sympathetic Nervous System
In our fast-paced modern society, stress has become a prevalent issue affecting many individuals. The constant pressure to meet deadlines, juggle multiple responsibilities, and navigate daily challenges can lead to chronic stress. This prolonged exposure to stressors can have a significant impact on the sympathetic nervous system.
Chronic stress can lead to continuous sympathetic activation, resulting in prolonged elevations in heart rate and blood pressure. The body remains in a state of heightened alertness, constantly prepared for potential threats. Over time, this sustained sympathetic dominance can have detrimental effects on cardiovascular health.
Research has shown that long-term sympathetic activation can contribute to the development of conditions such as hypertension, atherosclerosis, and heart disease. The constant strain on the heart and blood vessels can lead to structural changes and impair their function. Additionally, the increased production of stress hormones can disrupt the body’s delicate balance, further exacerbating the negative effects on cardiovascular health.
It is essential to recognize the impact of stress on the sympathetic nervous system and take steps to manage and reduce stress levels. Engaging in stress-reducing activities such as exercise, meditation, and spending time in nature can help restore balance and promote overall well-being.
The Parasympathetic Nervous System and Heart Rate
The parasympathetic nervous system acts as a counterbalance to the sympathetic activity, exerting a calming effect on heart rate and promoting relaxation.
The parasympathetic nervous system, also known as the “rest and digest” system, plays a crucial role in regulating heart rate. It works in opposition to the sympathetic nervous system, which is responsible for the body’s “fight or flight” response. While the sympathetic nervous system prepares the body for action and increases heart rate, the parasympathetic nervous system slows down heart rate and promotes a state of calmness.
When the parasympathetic nervous system is activated, it releases a neurotransmitter called acetylcholine. This neurotransmitter acts on specific receptors in the heart, slowing down the firing rate of pacemaker cells and reducing the force of contractions. As a result, the heart beats at a slower pace, allowing it to recover and conserve energy during periods of rest and recovery.
The Role of the Parasympathetic Nervous System in Heart Rate Control
Parasympathetic stimulation decreases heart rate by releasing acetylcholine, which acts on specific receptors in the heart, slowing down the firing rate of pacemaker cells and reducing the force of contractions. This allows the heart to recover and conserve energy during periods of rest and recovery.
Additionally, the parasympathetic nervous system also influences other aspects of heart function, such as regulating blood pressure and promoting healthy digestion. By activating the parasympathetic nervous system, the body can achieve a state of balance and optimal functioning.
It is important to note that the parasympathetic nervous system does not work in isolation. It works in conjunction with the sympathetic nervous system to maintain overall autonomic balance. When the body needs to respond to a stressful situation, the sympathetic nervous system takes over, increasing heart rate and preparing the body for action. However, once the threat has passed, the parasympathetic nervous system steps in to restore calmness and bring heart rate back to its resting state.
The Effect of Relaxation on the Parasympathetic Nervous System
Engaging in stress-management techniques, such as deep breathing exercises, meditation, or yoga, can activate the parasympathetic nervous system. This promotes a state of relaxation and helps restore autonomic balance, contributing to overall heart health.
During relaxation exercises, the body enters a state of calmness and tranquility. This triggers the release of neurotransmitters that activate the parasympathetic nervous system, leading to a decrease in heart rate. Deep breathing exercises, for example, stimulate the vagus nerve, a major component of the parasympathetic nervous system, which in turn releases acetylcholine and slows down heart rate.
Regular practice of relaxation techniques can have long-term benefits for heart health. By reducing stress and promoting relaxation, the parasympathetic nervous system is given the opportunity to function optimally, leading to improved heart rate control and overall cardiovascular well-being.
It is important to consult with a healthcare professional to determine the most appropriate relaxation techniques for individual needs. They can provide guidance on the best practices and help tailor a relaxation routine that suits specific health conditions and goals.
The Balance Between Sympathetic and Parasympathetic Activity
Maintaining a delicate balance between sympathetic and parasympathetic activity is vital for optimal heart health and overall well-being. The autonomic nervous system, which consists of the sympathetic and parasympathetic branches, plays a crucial role in regulating various bodily functions, including heart rate, blood pressure, and digestion.
The sympathetic branch of the autonomic nervous system is responsible for the “fight or flight” response. When activated, it prepares the body for action by increasing heart rate, constricting blood vessels, and releasing stress hormones like adrenaline. This response is essential in situations that require quick reactions, such as escaping from danger or intense physical exertion.
On the other hand, the parasympathetic branch of the autonomic nervous system promotes the “rest and digest” response. It helps the body relax, conserve energy, and restore balance after periods of stress or exertion. When activated, it slows down heart rate, dilates blood vessels, and enhances digestion and nutrient absorption.
The Importance of Autonomic Balance for Heart Health
Disruptions in the balance between sympathetic and parasympathetic activity can have adverse effects on the cardiovascular system. Imbalances, such as excessive sympathetic activation or diminished parasympathetic tone, are associated with increased risk of cardiovascular diseases, including hypertension, arrhythmias, and heart failure.
When sympathetic activity dominates, the heart may experience increased workload and oxygen demand, leading to elevated blood pressure and strain on the cardiovascular system. This can contribute to the development of conditions like hypertension, which is a significant risk factor for heart disease.
Conversely, reduced parasympathetic activity can impair the heart’s ability to recover and relax, hindering its ability to efficiently pump blood throughout the body. This can result in irregular heart rhythms, decreased cardiac output, and an increased risk of heart failure.
Factors Influencing Autonomic Balance
Various factors can impact the autonomic balance, including lifestyle choices, chronic stress, physical activity levels, and medical conditions. Unhealthy habits like smoking, excessive alcohol consumption, and a poor diet can disrupt the balance and negatively affect heart health.
Chronic stress, whether from work, relationships, or other sources, can also tip the scales towards sympathetic dominance. Prolonged activation of the sympathetic branch can lead to persistent high blood pressure, inflammation, and an increased risk of cardiovascular disease.
Engaging in regular physical activity, on the other hand, can help restore autonomic balance. Exercise has been shown to increase parasympathetic activity, promoting heart rate variability and improving overall cardiovascular function. Additionally, regular exercise can help reduce stress, enhance mood, and support healthy blood pressure levels.
It is important to note that certain medical conditions, such as diabetes, heart disease, and autonomic neuropathy, can disrupt the autonomic balance. These conditions may require specific interventions and management strategies to restore equilibrium and maintain heart health.
In conclusion, maintaining a balance between sympathetic and parasympathetic activity is crucial for optimal heart health. By adopting a healthy lifestyle, managing stress, and engaging in regular physical activity, individuals can support autonomic balance and reduce the risk of cardiovascular diseases. Consultation with a healthcare professional can provide personalized recommendations and guidance for maintaining a healthy autonomic nervous system.
The Clinical Implications of Autonomic Imbalance
An autonomic imbalance can have significant clinical implications for cardiovascular health. Understanding these implications can aid in the diagnosis and management of various cardiac conditions.
The autonomic nervous system plays a crucial role in regulating the functions of the cardiovascular system. It consists of two branches: the sympathetic nervous system, responsible for the “fight or flight” response, and the parasympathetic nervous system, responsible for the “rest and digest” response. When these two branches are in balance, the cardiovascular system functions optimally.
Autonomic Imbalance and Cardiovascular Disease
Research has shown that autonomic imbalance, characterized by sympathetic overactivation and parasympathetic underactivity, is associated with increased cardiovascular morbidity and mortality. This imbalance can lead to a range of cardiovascular diseases, including hypertension, arrhythmias, and heart failure.
Hypertension, or high blood pressure, is a common consequence of autonomic imbalance. Sympathetic overactivation can cause vasoconstriction, leading to increased peripheral resistance and elevated blood pressure. This chronic elevation in blood pressure puts a strain on the heart and blood vessels, increasing the risk of heart attack, stroke, and other cardiovascular events.
Arrhythmias, or abnormal heart rhythms, can also result from autonomic imbalance. The sympathetic nervous system stimulates the heart to beat faster and with more force, while the parasympathetic nervous system slows down the heart rate. When there is an imbalance between these two branches, it can disrupt the normal electrical signals in the heart, leading to arrhythmias such as atrial fibrillation or ventricular tachycardia.
In addition, autonomic imbalance can contribute to the development and progression of heart failure. The sympathetic overactivation causes the heart to work harder, leading to increased myocardial oxygen demand and potential damage to the heart muscle. Over time, this can weaken the heart and impair its ability to pump blood effectively.
Therapeutic Approaches for Autonomic Imbalance
Several therapeutic approaches aim to restore autonomic balance, including pharmacological interventions, lifestyle modifications, and targeted therapies. The choice of treatment depends on the underlying cause of the autonomic imbalance and the specific needs of the individual.
Pharmacological interventions can help modulate the activity of the autonomic nervous system. Beta-blockers, for example, can block the effects of sympathetic overactivation, reducing heart rate and blood pressure. On the other hand, cholinergic agents can enhance parasympathetic activity, promoting relaxation and reducing heart rate.
Lifestyle modifications also play a crucial role in managing autonomic imbalance. Regular exercise, a healthy diet, stress reduction techniques, and adequate sleep can all contribute to restoring autonomic balance. These lifestyle changes can help reduce sympathetic overactivation and promote parasympathetic activity, leading to improved cardiovascular health.
In some cases, targeted therapies may be necessary to address specific underlying causes of autonomic imbalance. For example, if an individual has an underlying medical condition such as diabetes or thyroid dysfunction that is contributing to the imbalance, treating the underlying condition can help restore autonomic balance.
It is important to note that the management of autonomic imbalance requires a comprehensive and individualized approach. A healthcare professional, such as a cardiologist or a neurologist, can assess the specific needs of each patient and develop a personalized treatment plan. Regular monitoring and follow-up are essential to ensure the effectiveness of the chosen therapeutic approaches and to make any necessary adjustments.
Conclusion
The regulation of heart rate involves the intricate interplay between the sympathetic and parasympathetic branches of the autonomic nervous system. The sympathetic division increases heart rate in response to stress or physical demands, while the parasympathetic division decreases heart rate, promoting relaxation and recovery. Maintaining a balance between sympathetic and parasympathetic activity is crucial for optimal heart health. Adopting a healthy lifestyle, managing stress, and seeking appropriate medical guidance are vital in promoting autonomic balance and ensuring cardiovascular well-being.