The parasympathetic nervous system plays a crucial role in regulating the activities of the heart. Understanding the intricate workings of this system and its impact on heart function is essential in comprehending various cardiac conditions and potential therapeutic approaches. In this comprehensive overview, we will delve into the fundamentals of the parasympathetic nervous system, explore its relationship with the heart, and examine the clinical implications and future directions of parasympathetic heart research.
Understanding the Parasympathetic Nervous System
The parasympathetic nervous system is one of the two major divisions of the autonomic nervous system, along with the sympathetic nervous system. While the sympathetic system primarily prepares the body for fight-or-flight responses, the parasympathetic system serves as the counterpart, responsible for promoting relaxation and maintaining homeostasis. It exerts its influence through a vast network of nerves spread throughout the body, including the heart.
The parasympathetic nervous system plays a crucial role in maintaining the body’s overall well-being. It acts as a balancing force, counteracting the effects of the sympathetic system to ensure that the body remains in a state of equilibrium. This delicate balance is essential for optimal functioning and health.
When the body is under stress or facing a threat, the sympathetic nervous system kicks into action, preparing the body for action. It increases heart rate, dilates blood vessels, and redirects blood flow to the muscles, enabling quick and efficient responses. However, once the threat has passed, the parasympathetic system takes over, bringing the body back to a state of calm and rest.
The Role of the Parasympathetic Nervous System
The primary role of the parasympathetic nervous system in relation to the heart is to slow down the heart rate, decrease the force of cardiac contractions, and promote coronary artery vasodilation. By doing so, it helps conserve energy and allows the heart to adapt to the body’s demands.
When the parasympathetic system is activated, it releases acetylcholine, a neurotransmitter that binds to specific receptors in the heart. This binding triggers a cascade of events that ultimately leads to a decrease in heart rate and a relaxation of the cardiac muscles. As a result, the heart beats at a slower pace, allowing for efficient blood flow and reduced strain on the cardiovascular system.
Furthermore, the parasympathetic system promotes coronary artery vasodilation, which increases blood flow to the heart muscle itself. This ensures that the heart receives an adequate supply of oxygen and nutrients, supporting its overall health and function.
Components of the Parasympathetic Nervous System
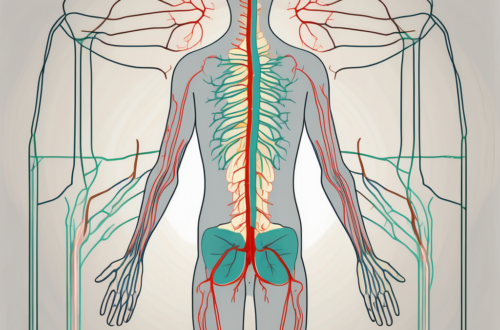
The key components of the parasympathetic nervous system involved in regulating heart function are the vagus nerves. These paired cranial nerves, also known as the tenth cranial nerves, originate in the brainstem and innervate various organs, including the heart. They contain fibers that release acetylcholine, a neurotransmitter that interacts with specific receptors in the heart to exert its parasympathetic effects.
The vagus nerves are responsible for transmitting signals from the brain to the heart, providing precise control over heart rate and contractility. Through their extensive network of fibers, they ensure that the parasympathetic effects are distributed evenly throughout the heart, allowing for coordinated and efficient cardiac function.
In addition to their role in heart regulation, the vagus nerves also play a part in controlling other bodily functions, such as digestion, respiration, and even emotional responses. Their widespread influence highlights the interconnectedness of the parasympathetic system and its impact on overall well-being.
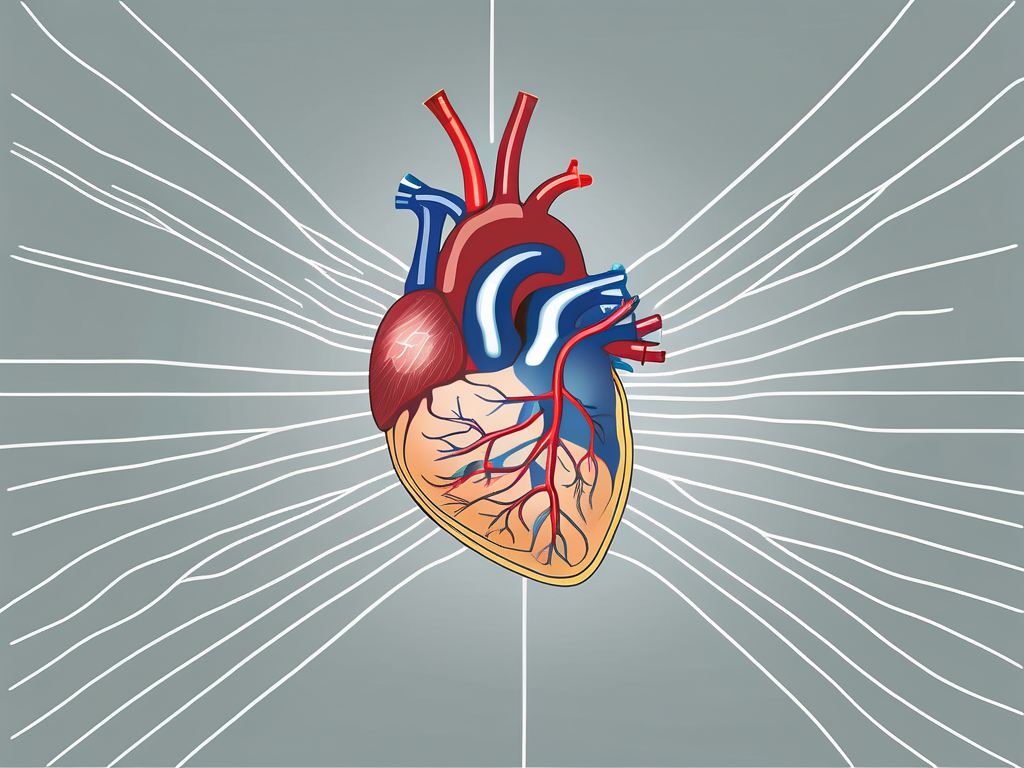
The Heart’s Parasympathetic Nerve Supply
The heart receives its parasympathetic nerve supply mainly through the vagus nerves. Understanding the anatomy and function of these nerves is crucial in comprehending their influence on heart health and disease.
The vagus nerves, also known as the tenth cranial nerves, are the longest and most complex of the cranial nerves. They originate from the medulla oblongata in the brainstem and travel a complex path down the neck and chest, ultimately reaching the heart. These nerves are responsible for transmitting parasympathetic signals to various organs in the body, including the heart.
As the vagus nerves approach the heart, they branch out extensively, forming intricate connections with cardiac structures. One of the key structures they interact with is the sinoatrial (SA) node, often referred to as the heart’s natural pacemaker. The SA node is responsible for initiating electrical impulses that regulate the heart’s rhythm. The parasympathetic nerve fibers within the vagus nerves release acetylcholine, a neurotransmitter that binds to muscarinic receptors primarily located in the SA node.
When acetylcholine binds to these receptors, it inhibits the generation of electrical impulses, effectively slowing down the heart rate. This parasympathetic influence helps maintain a steady and controlled heart rhythm, especially during periods of rest and relaxation. It counteracts the sympathetic nervous system’s effects, which are responsible for increasing heart rate and preparing the body for physical activity or stress.
In addition to its effects on the SA node, the parasympathetic nerve supply also influences the atrioventricular (AV) node. The AV node acts as a relay station, transmitting electrical signals from the atria to the ventricles. Acetylcholine released by the vagus nerves binds to muscarinic receptors in the AV node, slowing down the conduction of electrical impulses. This delay allows for proper coordination between atrial and ventricular contractions, ensuring efficient blood flow through the heart.
Furthermore, the parasympathetic nerve supply plays a role in regulating blood flow to the heart itself. Acetylcholine released by the vagus nerves promotes the relaxation of smooth muscles in the coronary arteries, which are responsible for supplying oxygenated blood to the heart muscle. This relaxation increases the diameter of the coronary arteries, allowing for improved blood flow and enhanced delivery of oxygen and nutrients to the heart.
In summary, the parasympathetic nerve supply to the heart, primarily through the vagus nerves, plays a crucial role in regulating heart rate, coordinating electrical conduction, and ensuring adequate blood supply to the heart muscle. Understanding the intricate anatomy and function of these nerves provides valuable insights into the mechanisms underlying heart health and disease.
The Vagus Nerve and the Heart
The vagus nerve, also referred to as the pneumogastric nerve, plays a pivotal role in mediating the parasympathetic effects on heart function.
The vagus nerve is a fascinating cranial nerve that extends throughout the body, making it the longest cranial nerve in the human body. It consists of both sensory and motor fibers, allowing it to carry information from various organs, including the heart, back to the brain. This nerve plays a vital role in regulating various bodily functions, such as digestion, respiration, and heart rate control.
The Vagus Nerve: An Overview
The vagus nerve, often referred to as the “wandering nerve,” gets its name from its extensive network of branches that reach out to different parts of the body. It originates in the medulla oblongata, which is located at the base of the brainstem, and travels down through the neck, chest, and abdomen, connecting to various organs along the way.
As the vagus nerve travels through the body, it collects sensory information from organs such as the heart and sends it back to the brain for processing. This information allows the brain to constantly monitor the state of the body and make necessary adjustments to maintain homeostasis.
The Vagus Nerve’s Influence on Heart Function
One of the most significant roles of the vagus nerve is its influence on heart function. The vagus nerve exerts its effects on the heart primarily through the release of a neurotransmitter called acetylcholine.
When acetylcholine binds to specific receptors in the heart, known as muscarinic receptors, it inhibits the activity of the sinoatrial (SA) and atrioventricular (AV) nodes. These nodes are responsible for initiating and regulating the electrical signals that control heart rate and conduction velocity.
By inhibiting the SA and AV nodes, the vagus nerve slows down the heart rate and reduces the conduction of electrical impulses through the heart. This parasympathetic influence helps to maintain a steady and controlled heart rhythm, especially during periods of rest and relaxation.
In addition to its effects on heart rate and conduction, the vagus nerve also plays a role in regulating blood flow to the heart. The vagus nerve’s impact on coronary artery smooth muscles leads to increased blood flow and improved cardiac oxygenation. This ensures that the heart receives an adequate supply of oxygen and nutrients to support its continuous pumping action.
Overall, the vagus nerve’s intricate connection with the heart highlights its crucial role in maintaining cardiovascular health. Its ability to modulate heart rate, conduction, and blood flow demonstrates the complex interplay between the nervous system and the cardiovascular system.
Parasympathetic Control of Heart Rate
The parasympathetic nervous system plays a crucial role in maintaining heart rate homeostasis. Understanding the mechanisms underlying parasympathetic control and its impact on heart rate can provide insight into various cardiac conditions.
The parasympathetic control of heart rate primarily occurs through the vagus nerves, which release acetylcholine to bind with muscarinic receptors in the heart. This binding inhibits the activity of the SA node, the natural pacemaker of the heart, slowing down the heart rate.
Additionally, parasympathetic control of heart rate involves the activation of the atrioventricular (AV) node. The AV node acts as a relay station, receiving signals from the SA node and transmitting them to the ventricles. When the parasympathetic nervous system is activated, it releases acetylcholine, which binds to muscarinic receptors in the AV node. This binding slows down the conduction of electrical signals through the AV node, further reducing the heart rate.
Furthermore, parasympathetic control of heart rate is influenced by the baroreceptor reflex. Baroreceptors are specialized sensory receptors located in the walls of the major blood vessels. They detect changes in blood pressure and send signals to the brainstem, which then activates the parasympathetic nervous system. This activation leads to a decrease in heart rate, helping to regulate blood pressure and maintain cardiovascular homeostasis.
Parasympathetic control contributes significantly to heart rate variability and allows the heart to adapt to changing physiological demands. In situations where increased parasympathetic activity is required, such as during rest or relaxation, heart rate decreases. This decrease in heart rate promotes a state of calmness and relaxation, conserving energy and promoting recovery.
However, excessive parasympathetic stimulation can lead to bradycardia, an abnormally slow heart rate. Bradycardia can be caused by various factors, including certain medications, heart diseases, and dysfunction of the autonomic nervous system. It can result in symptoms such as fatigue, dizziness, and fainting, and may require medical intervention to restore a normal heart rate.
In conclusion, the parasympathetic nervous system plays a vital role in the control of heart rate. Through the release of acetylcholine and activation of muscarinic receptors, parasympathetic stimulation slows down the activity of the SA node and the AV node, leading to a decrease in heart rate. This control mechanism allows the heart to adapt to different physiological demands and maintain cardiovascular homeostasis. However, excessive parasympathetic stimulation can have detrimental effects and lead to bradycardia. Further research in this field can help unravel the complexities of parasympathetic control and its implications for cardiac health.
Clinical Implications of Parasympathetic Nerve Supply
The parasympathetic nerve supply of the heart has significant clinical implications, especially in the context of heart disease. Understanding these implications is crucial for medical professionals to provide optimal care to patients.
When it comes to the parasympathetic nerve supply in heart disease, there is a complex interplay between various cardiac conditions and the balance between the parasympathetic and sympathetic nervous systems. In conditions such as heart failure, myocardial infarction, and arrhythmias, this delicate balance may become disrupted, leading to adverse effects on heart rate, conduction, and contractility. These effects can contribute to the progression of the disease and impact patient outcomes.
Heart failure, for example, is a condition characterized by the heart’s inability to pump blood effectively. In this condition, the parasympathetic nervous system’s activity may be reduced, while the sympathetic nervous system’s activity is increased. This imbalance can lead to increased heart rate, impaired contractility, and abnormal conduction, further compromising the heart’s function.
Similarly, in the case of myocardial infarction, commonly known as a heart attack, the disruption of the parasympathetic nerve supply can have detrimental effects. During a heart attack, the blood supply to a part of the heart is blocked, leading to tissue damage. This damage can affect the parasympathetic nerve fibers, resulting in an imbalance between the two autonomic divisions. The altered parasympathetic activity can contribute to arrhythmias and further compromise the heart’s ability to function properly.
Recognizing the importance of the parasympathetic nerve supply in heart disease, medical professionals have developed various therapeutic approaches to modulate its activity. Medications that enhance or suppress parasympathetic activity, such as beta-blockers and cholinergic drugs, have been used to restore the balance between the autonomic divisions. These medications can help regulate heart rate, improve contractility, and reduce the risk of arrhythmias.
In addition to pharmacological interventions, other innovative approaches have emerged to target the parasympathetic nerve supply. Vagus nerve stimulation, for example, involves the use of electrical impulses to activate the parasympathetic fibers of the vagus nerve. This technique has shown promising results in managing heart failure and arrhythmias by restoring the balance between the autonomic divisions.
Researchers are also exploring novel interventions aimed at restoring the parasympathetic-sympathetic balance in heart disease. These interventions may involve targeted gene therapy, stem cell transplantation, or the development of bioengineered tissues that can integrate with the damaged heart tissue and promote parasympathetic nerve regeneration.
In conclusion, the parasympathetic nerve supply plays a crucial role in heart function and has significant clinical implications in the context of heart disease. Understanding the complex interplay between the parasympathetic and sympathetic nervous systems can help medical professionals provide optimal care to patients. With ongoing research and the development of innovative therapeutic approaches, there is hope for improving outcomes and quality of life for individuals with heart disease.
Future Directions in Parasympathetic Heart Research
As technology advances and our understanding of the parasympathetic nerve supply expands, exciting research opportunities emerge. These avenues of exploration have the potential to revolutionize heart health and treatment strategies.
The parasympathetic nervous system plays a crucial role in regulating the heart’s functions, including heart rate, blood pressure, and overall cardiac health. By further investigating the intricacies of this system, researchers hope to uncover new insights that can lead to groundbreaking advancements in cardiovascular medicine.
Emerging Research Trends
Ongoing research explores innovative ways to modulate the parasympathetic nerve supply, such as targeted drug delivery systems and bioelectronic medicine approaches. These cutting-edge technologies aim to precisely regulate the parasympathetic activity, providing a more targeted and effective treatment for various cardiac conditions.
Furthermore, studies are being conducted to elucidate the interplay between the parasympathetic and sympathetic systems. By understanding how these two branches of the autonomic nervous system interact, researchers can gain a deeper understanding of the complex mechanisms that control heart function. This knowledge may open doors to novel therapeutic approaches that can optimize autonomic control and improve cardiac health outcomes.
Potential Innovations in Heart Health and Treatment
The future of parasympathetic heart research holds promise for the development of advanced therapeutic options. These may include personalized medicine approaches, interventions harnessing the body’s natural mechanisms, and innovative strategies aimed at optimizing the delicate balance between the autonomic divisions.
Personalized medicine approaches take into account an individual’s unique genetic makeup, lifestyle factors, and medical history to tailor treatment plans specifically to their needs. By incorporating parasympathetic heart research findings, healthcare providers can offer more precise and effective interventions that address the root causes of cardiac disorders.
In addition, interventions that harness the body’s natural mechanisms are being explored. These interventions aim to enhance the parasympathetic activity through non-invasive techniques such as meditation, deep breathing exercises, and acupuncture. By activating the body’s own healing mechanisms, these approaches have the potential to improve heart health and overall well-being.
Collaborative efforts between scientists, clinicians, and technology experts pave the way for exciting breakthroughs in parasympathetic heart research. By combining expertise from various fields, researchers can develop innovative strategies and technologies that have the potential to transform the landscape of cardiovascular medicine.
While this comprehensive overview provides valuable insights into the parasympathetic nerve supply of the heart, it is crucial to consult with a healthcare professional for personalized advice and guidance. Understanding the complexities of parasympathetic heart regulation empowers both patients and healthcare providers in their journey towards optimal cardiac wellness.