The parasympathetic nerve plays a crucial role in the functioning of the thoracic viscera. Understanding the intricacies of this nerve system is essential for comprehending its impact on various organs within the thoracic cavity. This article aims to shed light on the anatomy, function, potential dysfunctions, and treatment options associated with the parasympathetic nerve in thoracic viscera.
Understanding the Parasympathetic Nervous System
The Anatomy and Function of the Parasympathetic Nerve
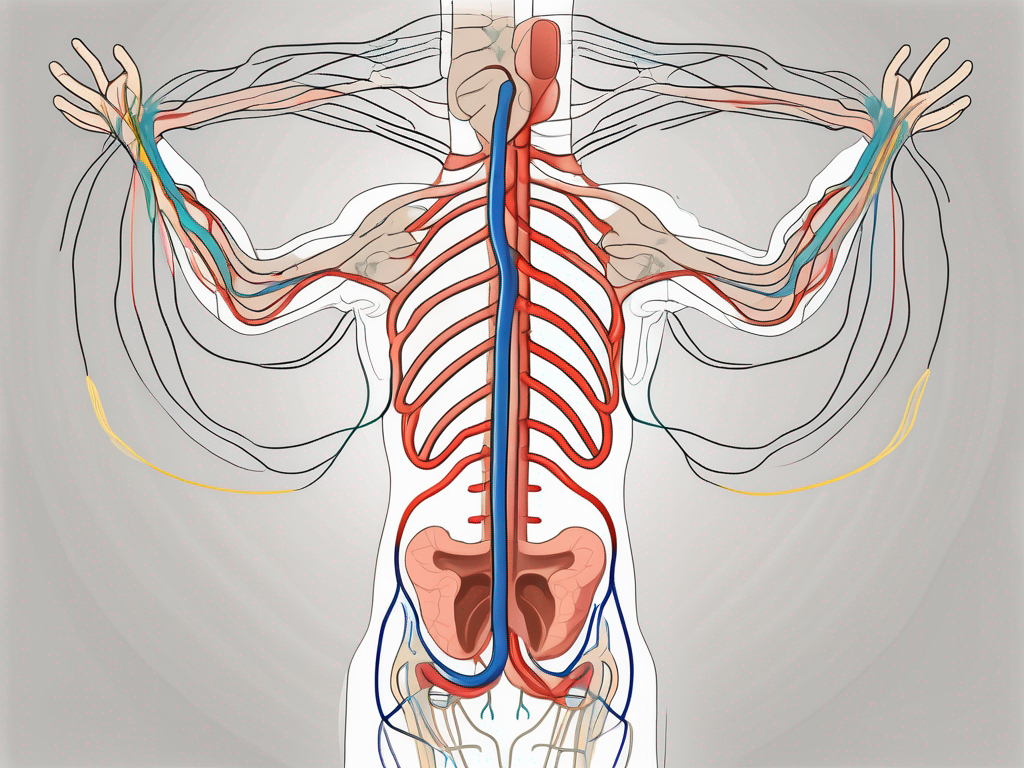
The parasympathetic nervous system is one of the two main divisions of the autonomic nervous system, alongside the sympathetic nervous system. It primarily functions to restore the body to a state of calm and relaxation, often referred to as the “rest and digest” response. The parasympathetic nerve fibers arise from the cranial nerves (specifically the vagus nerve) and the sacral nerves.
Within the thoracic viscera, the parasympathetic nerve exerts its influence on various organs, including the heart, lungs, and esophagus. By understanding the anatomical pathways and connectivity of the parasympathetic nerve, we can better comprehend its role in regulating these vital structures.
The vagus nerve, a major component of the parasympathetic nervous system, originates in the medulla oblongata of the brainstem. It extends down through the neck, chest, and abdomen, sending branches to multiple organs along the way. These branches innervate the heart, where they help regulate heart rate and cardiac output. They also reach the lungs, where they influence bronchial constriction and secretion production. Additionally, the vagus nerve plays a crucial role in controlling the muscles of the esophagus, aiding in the process of swallowing and preventing reflux.
In the sacral region, the parasympathetic nerve fibers emerge from the spinal cord and contribute to the regulation of pelvic organs. These fibers innervate the bladder, promoting detrusor muscle contraction for urination, while also inhibiting the sphincter muscles to allow for the smooth flow of urine. In the reproductive system, the parasympathetic nerve facilitates sexual arousal by increasing blood flow to the genital organs.
The Parasympathetic Nervous System and the Body’s Rest and Digest Response
When the parasympathetic nervous system is activated, it signals for the body to enter a state of relaxation and restoration. This response allows for optimal digestion, nutrient absorption, and overall physiological balance. The parasympathetic nerve stimulates the release of enzymes and increases blood flow to the gastrointestinal tract, facilitating digestion and nutrient uptake.
Moreover, the rest and digest response leads to a decrease in heart rate and blood pressure, promoting a sense of calmness and tranquility within the thoracic region. This justifies the importance of parasympathetic nerve function in maintaining healthy thoracic viscera.
Furthermore, the parasympathetic nervous system influences the function of the liver and pancreas. It stimulates the release of bile from the gallbladder, aiding in the digestion and absorption of fats. Additionally, it promotes the secretion of insulin from the pancreas, which helps regulate blood sugar levels. These actions highlight the extensive reach and impact of the parasympathetic nerve on various physiological processes.
Additionally, the parasympathetic nervous system plays a crucial role in the regulation of the ocular muscles. It controls the constriction of the pupils, allowing for proper focusing and adjustment to different lighting conditions. This intricate control ensures optimal vision and eye health.
In summary, the parasympathetic nervous system is a vital component of the autonomic nervous system, responsible for promoting relaxation, digestion, and overall physiological balance. Its extensive network of nerve fibers connects to various organs and structures, allowing for precise regulation and control. Understanding the intricacies of the parasympathetic nerve’s anatomy and function provides valuable insights into the body’s rest and digest response and its impact on overall health and well-being.
The Parasympathetic Nerve and Thoracic Viscera
The Parasympathetic Nerve’s Influence on the Heart
The parasympathetic nerve fibers that innervate the heart have a unique impact on cardiac function. Through the vagus nerve, the parasympathetic system slows down the heart rate, contributing to overall heart rate variability and regulation of cardiac output. This regulation is essential for maintaining a healthy cardiovascular system.
When the parasympathetic nerve is activated, it releases acetylcholine, which binds to receptors on the heart’s cells. This binding leads to a decrease in heart rate and the force of contraction. By slowing down the heart rate, the parasympathetic nerve allows the heart to rest and recover, ensuring efficient blood flow throughout the body.
However, dysfunction in this aspect of the parasympathetic nerve can lead to irregular heart rhythms or bradycardia, limiting the heart’s ability to pump effectively. In such cases, medical intervention may be necessary to restore proper cardiac function and prevent complications.
The Role of the Parasympathetic Nerve in Lung Function
In the realm of respiratory function, the parasympathetic nerve plays a crucial role in maintaining optimal lung function and airway constriction. It controls the constriction of bronchial smooth muscles, helping regulate airflow within the lungs.
When the parasympathetic nerve is stimulated, it causes the bronchial smooth muscles to contract, narrowing the airways. This constriction helps redirect airflow to specific areas of the lungs, ensuring efficient gas exchange. Additionally, the parasympathetic nerve also stimulates the production of mucus in the airways, which helps trap foreign particles and protect the lungs from potential harm.
However, dysfunction of the parasympathetic nerve in the lungs may result in conditions such as bronchospasm or respiratory distress. In these cases, the airways become overly constricted, making it difficult to breathe. Seeking prompt medical attention is crucial to manage and treat these conditions effectively.
The Parasympathetic Nerve and the Esophagus
Within the esophagus, the parasympathetic nerve fibers facilitate the movement of food down towards the stomach. These nerves stimulate the muscular contractions needed for smooth and efficient swallowing.
When food is swallowed, the parasympathetic nerve signals the muscles in the esophagus to contract in a coordinated manner, propelling the food downward. This process, known as peristalsis, ensures that food reaches the stomach safely and without any obstructions.
Disruptions in the function of the parasympathetic nerve in the esophagus may contribute to swallowing difficulties or conditions like gastroesophageal reflux disease (GERD). In GERD, the lower esophageal sphincter fails to close properly, allowing stomach acid to flow back into the esophagus, causing discomfort and potential damage. Seeking medical advice is advised to manage such concerns effectively and prevent complications.
The Impact of Parasympathetic Nerve Dysfunction
Parasympathetic nerve dysfunction can have a significant impact on the body, affecting various organs and systems within the thoracic viscera. Understanding the symptoms, signs, and potential causes of parasympathetic nerve dysfunction is crucial for proper diagnosis and treatment.
Symptoms and Signs of Parasympathetic Nerve Dysfunction
When the parasympathetic nerves are not functioning properly, it can manifest in a range of symptoms and signs. The specific indicators may vary depending on the affected organ or system within the thoracic viscera.
One common symptom of parasympathetic nerve dysfunction is irregular heart rhythms. This can lead to palpitations, a sensation of the heart racing or skipping beats, and may cause dizziness or lightheadedness.
Difficulty breathing is another potential sign of parasympathetic nerve dysfunction. The nerves responsible for controlling the muscles involved in respiration may be affected, leading to shortness of breath or a feeling of not getting enough air.
Gastrointestinal disturbances are also frequently associated with parasympathetic nerve dysfunction. These can include bloating, abdominal discomfort, indigestion, and changes in bowel movements.
In some cases, swallowing difficulties may arise due to impaired parasympathetic nerve function. This can make it challenging to eat and drink, potentially leading to weight loss or malnutrition if left untreated.
If you are experiencing persistent or concerning symptoms related to parasympathetic nerve dysfunction, it is crucial to seek medical evaluation. A healthcare professional can assess your condition, perform necessary tests, and recommend appropriate treatment options.
Potential Causes of Parasympathetic Nerve Dysfunction
Parasympathetic nerve dysfunction can have various underlying causes, ranging from medical conditions to lifestyle factors. Identifying the root cause is essential for developing an appropriate treatment plan.
Neurological disorders can contribute to parasympathetic nerve dysfunction. Conditions such as Parkinson’s disease, multiple system atrophy, and autonomic neuropathy can affect the nerves responsible for regulating parasympathetic function.
Trauma or injury to the nerves can also lead to dysfunction. Accidents, falls, or surgical procedures in the thoracic region may damage the parasympathetic nerves, disrupting their normal functioning.
Certain medications can interfere with parasympathetic nerve activity, leading to dysfunction. Drugs used to treat conditions like high blood pressure, depression, or urinary incontinence may have side effects that affect the parasympathetic system.
Chronic stress is another potential cause of parasympathetic nerve dysfunction. Prolonged periods of stress can disrupt the balance between the sympathetic and parasympathetic systems, impacting overall autonomic function.
If you suspect parasympathetic nerve dysfunction, it is important to consult with a healthcare professional. They can evaluate your symptoms, review your medical history, and perform any necessary tests to determine the underlying cause. With proper diagnosis, appropriate treatment options can be explored to manage and alleviate the symptoms associated with parasympathetic nerve dysfunction.
Treatment and Management of Parasympathetic Nerve Dysfunction
Parasympathetic nerve dysfunction can have a significant impact on an individual’s overall health and well-being. When dealing with this condition, it is important to explore various treatment options and make necessary lifestyle changes to support optimal nerve function.
Medical Interventions for Parasympathetic Nerve Dysfunction
When it comes to managing parasympathetic nerve dysfunction, medical interventions may be necessary depending on the specific condition and its severity. These interventions aim to address the underlying causes and alleviate symptoms that may be affecting an individual’s quality of life.
One common medical intervention for parasympathetic nerve dysfunction is the use of medications to regulate heart rate. This can help stabilize the autonomic nervous system and promote a more balanced functioning of the parasympathetic nervous system. Additionally, bronchodilators may be prescribed to improve lung function, especially in cases where respiratory symptoms are present.
In some cases, surgical procedures may be required to address nerve injuries or abnormalities that are contributing to parasympathetic nerve dysfunction. These procedures aim to repair or restore the affected nerves, allowing for improved nerve function and overall well-being.
It is crucial to consult with a healthcare professional to determine the most suitable intervention for individual circumstances. A thorough evaluation of symptoms, medical history, and diagnostic tests will help guide the treatment plan and ensure the best possible outcomes.
Lifestyle Changes to Support Parasympathetic Nerve Health
Alongside medical interventions, lifestyle changes can play a significant role in supporting optimal parasympathetic nerve function. These changes aim to create an environment that promotes nerve health and overall well-being.
One important lifestyle change is stress reduction techniques. Chronic stress can negatively impact the parasympathetic nervous system, leading to dysfunction. Engaging in activities such as meditation, deep breathing exercises, or yoga can help reduce stress levels and promote relaxation, ultimately supporting the health of the parasympathetic nerves.
Regular physical activity is another crucial aspect of supporting parasympathetic nerve health. Exercise helps improve blood circulation, oxygenation, and overall cardiovascular health, which in turn supports the optimal functioning of the parasympathetic nervous system. It is important to find an exercise routine that suits individual preferences and abilities, ensuring consistency and enjoyment.
Adopting a balanced diet is also essential for maintaining parasympathetic nerve health. A diet rich in fruits, vegetables, whole grains, and lean proteins provides the necessary nutrients and antioxidants to support nerve function. Avoiding excessive consumption of processed foods, sugary snacks, and caffeine can also contribute to a healthier nervous system.
Lastly, getting adequate sleep is crucial for overall well-being and parasympathetic nerve health. During sleep, the body repairs and rejuvenates itself, including the nervous system. Establishing a regular sleep routine and creating a relaxing sleep environment can help promote restful sleep and support optimal nerve function.
Prioritizing self-care and seeking ways to enhance overall well-being can contribute to the improvement of parasympathetic nerve health. It is important to remember that everyone’s journey towards optimal nerve function may be different, and a multidimensional approach that combines medical interventions and lifestyle changes is often the most effective way to manage parasympathetic nerve dysfunction.
Future Research Directions in Parasympathetic Nerve Function
Emerging Technologies in Parasympathetic Nerve Study
The scientific community is continuously exploring new technologies to enhance our understanding of the parasympathetic nerve and its role in thoracic viscera. Emerging technologies such as neuroimaging techniques, electrophysiological recordings, and advancements in molecular biology provide promising avenues for unraveling further intricacies surrounding this vital nerve system.
Neuroimaging techniques, such as functional magnetic resonance imaging (fMRI), have revolutionized the field of neuroscience. These imaging tools allow researchers to visualize the activity of the parasympathetic nerve in real-time, providing valuable insights into its function and connectivity with other regions of the brain. By studying the patterns of neural activation, scientists can better understand how the parasympathetic nerve influences various thoracic organs.
In addition to neuroimaging, electrophysiological recordings have become increasingly sophisticated, enabling researchers to measure the electrical activity of the parasympathetic nerve with high precision. Techniques such as electroencephalography (EEG) and nerve conduction studies provide valuable information about the timing and strength of nerve signals, shedding light on the underlying mechanisms of parasympathetic nerve function.
Advancements in molecular biology have also contributed to our understanding of the parasympathetic nerve. Researchers can now study the genetic and molecular components of this nerve system, identifying specific genes and proteins that play a crucial role in its development and function. By manipulating these molecular pathways, scientists hope to uncover new therapeutic targets for treating parasympathetic nerve dysfunction.
Unanswered Questions in Parasympathetic Nerve Research
Despite significant progress in parasympathetic nerve research, numerous questions remain unanswered. Researchers are actively investigating the specific mechanisms underlying parasympathetic nerve dysfunction and exploring novel therapeutic targets. Understanding the fundamental aspects of parasympathetic nerve biology and its impact on thoracic viscera will enable future advancements in the diagnosis and treatment of related conditions.
One of the key unanswered questions in parasympathetic nerve research is how the nerve system regulates the functioning of different thoracic organs. While it is known that the parasympathetic nerve influences the heart, lungs, and esophagus, the precise mechanisms by which it exerts its control are still not fully understood. Further research is needed to elucidate the intricate pathways and signaling molecules involved in these processes.
Another area of interest is the role of the parasympathetic nerve in disease states. Researchers are investigating how parasympathetic nerve dysfunction contributes to conditions such as gastroesophageal reflux disease (GERD), asthma, and arrhythmias. By understanding the specific alterations in parasympathetic nerve activity in these diseases, scientists can develop targeted interventions to alleviate symptoms and improve patient outcomes.
Furthermore, the impact of lifestyle factors on parasympathetic nerve function is an area of ongoing investigation. Researchers are exploring how factors such as stress, diet, and physical activity influence the activity and responsiveness of the parasympathetic nerve. By identifying modifiable lifestyle factors that can positively impact parasympathetic nerve function, interventions can be developed to promote overall health and well-being.
In conclusion, the parasympathetic nerve plays a critical role in the functioning of thoracic viscera. Its influence on various organs such as the heart, lungs, and esophagus highlights the necessity for proper function within the parasympathetic nervous system. Identifying symptoms, understanding potential causes, and seeking appropriate medical care are essential steps in managing parasympathetic nerve dysfunction. As research continues to advance, new insights into this intricate nerve system will pave the way for improved diagnostics and targeted treatments.