Beta cells, a key component of the endocrine pancreas, play a crucial role in maintaining glucose homeostasis in the body. Their function is regulated by a multitude of factors, including the parasympathetic nervous system. Understanding the intricate interplay between the parasympathetic nerve and beta cells is essential for unraveling the mechanisms underlying glucose regulation. In this article, we will explore the anatomy and function of the parasympathetic nervous system, delve into the importance of beta cells, examine the interaction between the parasympathetic nerve and beta cells, discuss potential health implications, and explore future directions in parasympathetic nerve and beta cell research.
Understanding the Parasympathetic Nervous System
The parasympathetic nervous system is one of the two main divisions of the autonomic nervous system, along with the sympathetic nervous system. Its primary function is to restore and conserve energy by promoting rest, digestion, and relaxation. Unlike the sympathetic nervous system, which prepares the body for action and stress, the parasympathetic nervous system is responsible for counterbalancing these effects and maintaining a state of equilibrium.
When we think about the parasympathetic nervous system, it’s important to understand its intricate anatomy and how it functions to regulate various bodily processes. Let’s dive deeper into the fascinating world of the parasympathetic nervous system.
The Anatomy of the Parasympathetic Nervous System
The parasympathetic nervous system consists of cranial and sacral outflow pathways. The cranial outflow originates from the brainstem and includes the vagus nerve (cranial nerve X), which innervates various organs in the chest, abdomen, and pelvis. This intricate network of nerves allows for precise control over vital functions such as heart rate, digestion, and glandular secretion.
On the other hand, the sacral outflow originates from the sacral spinal cord and innervates the lower parts of the gastrointestinal and genitourinary systems. This division of the parasympathetic nervous system plays a crucial role in regulating processes like urination, defecation, and sexual function.
Together, these two pathways work harmoniously to ensure the proper functioning of different organs and tissues in the body. It’s truly remarkable how the parasympathetic nervous system orchestrates such intricate processes.
The Function of the Parasympathetic Nervous System
The parasympathetic nervous system regulates several vital functions, including heart rate, digestion, and glandular secretion. When activated, it promotes a state of rest and relaxation, allowing the body to conserve and restore energy. This is crucial for maintaining overall well-being and ensuring the body’s optimal functioning.
One of the primary ways in which the parasympathetic nervous system exerts its effects is through the release of acetylcholine, a neurotransmitter that binds to specific receptors on target cells, initiating a cascade of physiological responses. This intricate signaling system allows for precise control over various bodily processes, ensuring that everything runs smoothly.
For example, when the parasympathetic nervous system is activated, it slows down the heart rate, allowing the body to relax. It also stimulates digestion, promoting the breakdown of food and absorption of nutrients. Additionally, it enhances glandular secretion, ensuring the proper functioning of glands throughout the body.
Understanding the parasympathetic nervous system is essential for comprehending the delicate balance that exists within our bodies. It’s incredible how this intricate system works tirelessly to maintain equilibrium and keep us functioning optimally.
So, the next time you find yourself in a state of relaxation or enjoying a delicious meal, remember to thank your parasympathetic nervous system for its remarkable work!
The Importance of Beta Cells
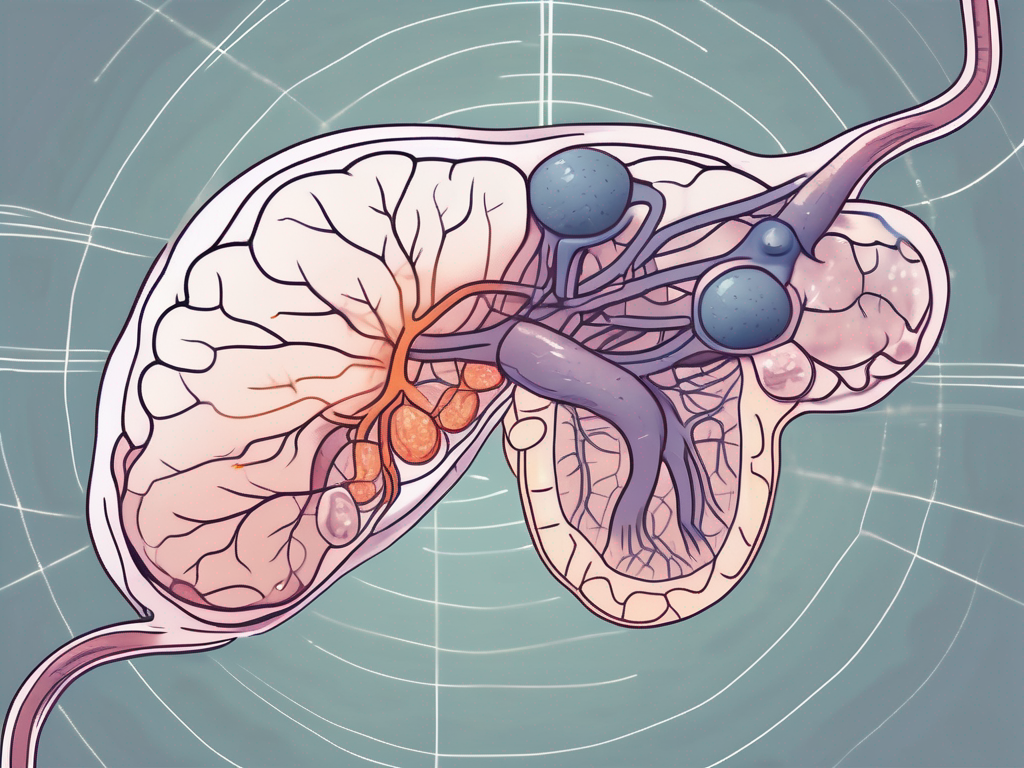
Beta cells are specialized cells located within the islets of Langerhans in the pancreas. They constitute approximately 60-80% of the total islet cell population and are responsible for producing and releasing insulin, a hormone that regulates blood glucose levels. Insulin is essential for facilitating the uptake of glucose from the bloodstream into the body’s cells, where it is used as a source of energy. Without properly functioning beta cells, the body’s ability to regulate glucose levels is compromised, leading to a range of health issues.
The Structure of Beta Cells
Beta cells are characterized by their unique cellular structure. They possess granules known as insulin secretory granules, which are enriched with insulin molecules. These granules are released into the bloodstream in response to various physiological stimuli, such as elevated blood glucose levels. Beta cells are also equipped with specialized ion channels and transporters that allow them to sense changes in glucose concentration and regulate insulin secretion accordingly.
Furthermore, beta cells have a distinct morphology that sets them apart from other cell types in the pancreas. They are typically larger in size and have a higher number of mitochondria, which are responsible for producing the energy needed for insulin synthesis and secretion. This increased mitochondrial density reflects the high metabolic demands placed on beta cells to maintain glucose homeostasis.
The Role of Beta Cells in Glucose Regulation
Beta cells play a crucial role in maintaining glucose homeostasis in the body. When blood glucose levels rise, beta cells respond by secreting insulin into the bloodstream, which helps to lower glucose levels by promoting its uptake into cells. This process is tightly regulated to prevent excessive insulin secretion, which could lead to hypoglycemia.
Moreover, beta cells not only respond to changes in glucose levels but also integrate signals from other hormones and nutrients to fine-tune insulin secretion. For example, incretin hormones released from the intestines in response to food intake enhance beta cell function and insulin release. This complex interplay between beta cells and various factors ensures that glucose regulation is finely tuned to meet the body’s metabolic needs.
Additionally, beta cells exhibit remarkable plasticity, meaning they can adapt and change their function in response to different physiological conditions. For instance, during pregnancy, beta cells undergo a process called hyperplasia, where their numbers increase to meet the increased demand for insulin. This adaptive response ensures that the mother’s glucose levels remain within the normal range, supporting the growth and development of the fetus.
In conclusion, beta cells are a vital component of the pancreas and play a crucial role in maintaining glucose homeostasis. Their unique structure, ability to sense glucose levels, and plasticity make them essential for regulating blood glucose levels and preventing the development of metabolic disorders. Understanding the importance of beta cells provides valuable insights into the complex mechanisms underlying glucose regulation and opens avenues for developing novel therapeutic strategies to treat diabetes and related conditions.
The Interaction between the Parasympathetic Nerve and Beta Cells
The parasympathetic nervous system, through its intricate neural connections, exerts a significant influence on beta cell function and glucose regulation. The activation of parasympathetic pathways stimulates beta cells to release insulin, thereby promoting glucose uptake and storage. Conversely, the inhibition of parasympathetic activity diminishes insulin secretion and impairs glucose utilization. This dynamic interplay between the parasympathetic nerve and beta cells is essential for maintaining glucose homeostasis.
Glucose homeostasis, the balance between glucose production and utilization, is a tightly regulated process in the body. The parasympathetic nervous system plays a crucial role in this regulation by directly influencing the activity of beta cells, which are responsible for insulin secretion. Insulin, in turn, is the key hormone involved in glucose uptake and storage.
When the parasympathetic nervous system is activated, it stimulates beta cells to release insulin. This activation occurs through the release of acetylcholine, a neurotransmitter that binds to specific receptors on beta cells. The binding of acetylcholine triggers a series of cellular events within the beta cells, ultimately leading to the secretion of insulin. This insulin release promotes the uptake of glucose by various tissues, such as skeletal muscle and adipose tissue, and facilitates its storage as glycogen or fat.
Conversely, when the parasympathetic activity is inhibited, insulin secretion is diminished, leading to impaired glucose utilization. This inhibition can occur in response to various factors, such as stress or sympathetic nervous system activation. In these situations, the body prioritizes other physiological processes over glucose regulation, resulting in a decrease in insulin secretion and a rise in blood glucose levels.
The Impact of the Parasympathetic Nerve on Beta Cell Activity
Activation of the parasympathetic nervous system stimulates beta cells to release insulin, primarily through the release of acetylcholine. This neurotransmitter binds to specific receptors on beta cells, triggering a series of cellular events that culminate in insulin secretion. By enhancing beta cell activity, the parasympathetic nerve ensures efficient glucose regulation and helps maintain optimal blood glucose levels.
The parasympathetic nerve’s impact on beta cell activity is not limited to insulin secretion alone. It also influences other aspects of beta cell function, such as the synthesis and processing of insulin. Studies have shown that parasympathetic stimulation can increase the expression of genes involved in insulin production and promote the proper folding and packaging of insulin molecules within beta cells. These processes are essential for the efficient production and release of functional insulin.
Furthermore, the parasympathetic nervous system can also modulate the sensitivity of beta cells to glucose. It has been observed that parasympathetic activation enhances the responsiveness of beta cells to changes in blood glucose levels, allowing for a more precise and rapid adjustment of insulin secretion. This fine-tuning of beta cell sensitivity helps maintain glucose homeostasis and prevents excessive fluctuations in blood glucose levels.
The Influence of Beta Cells on Parasympathetic Nerve Function
Beta cells also have a reciprocal relationship with the parasympathetic nervous system. Insulin, in addition to its role in glucose regulation, can influence the activity of the parasympathetic nerve. Studies have shown that insulin can modulate parasympathetic activity, highlighting the bidirectional influence between beta cells and the parasympathetic nervous system. This interplay may have implications for various physiological processes beyond glucose regulation.
Insulin receptors are present on parasympathetic nerve fibers, suggesting that insulin can directly affect their function. Research has demonstrated that insulin can enhance parasympathetic activity, leading to increased vagal tone. Vagal tone refers to the activity of the vagus nerve, a major component of the parasympathetic nervous system, and is associated with various physiological functions, including heart rate regulation and digestion.
Additionally, insulin has been found to modulate the release of neurotransmitters within the parasympathetic nervous system. It can influence the synthesis and release of acetylcholine, the primary neurotransmitter involved in parasympathetic signaling. By regulating neurotransmitter release, insulin can indirectly impact the overall activity of the parasympathetic nervous system and its effects on various target tissues.
Overall, the interaction between beta cells and the parasympathetic nerve is a complex and dynamic process. The parasympathetic nervous system stimulates beta cells to release insulin, promoting glucose uptake and storage. In turn, insulin can influence parasympathetic activity, further modulating its effects on various physiological processes. This bidirectional interaction highlights the intricate relationship between the parasympathetic nervous system and beta cells in maintaining glucose homeostasis and overall physiological balance.
Potential Health Implications of Parasympathetic Nerve-Beta Cell Interactions
The intricate interactions between the parasympathetic nerve and beta cells have significant implications for overall health and disease states. Dysregulation of these interactions can contribute to the development of conditions such as diabetes mellitus, a chronic metabolic disorder characterized by impaired glucose regulation. Understanding the underlying mechanisms of parasympathetic nerve-beta cell interactions in health and disease can pave the way for novel therapeutic interventions.
When it comes to the parasympathetic nerve and beta cells, their interactions are crucial for maintaining proper glucose regulation in the body. The parasympathetic nervous system, often referred to as the “rest and digest” system, plays a vital role in promoting digestion and regulating various bodily functions. Beta cells, on the other hand, are responsible for producing and releasing insulin, a hormone that helps regulate blood sugar levels.
In diabetes, the delicate balance between the parasympathetic nerve and beta cells is disrupted, leading to abnormal glucose regulation. Dysfunction of the parasympathetic nervous system can impair insulin secretion and exacerbate hyperglycemia, a hallmark of diabetes. Similarly, impaired beta cell function can hinder parasympathetic activity and perturb glucose homeostasis. This intricate interplay between the parasympathetic nerve and beta cells highlights the importance of addressing both factors in managing and treating diabetes.
The Role of Parasympathetic Nerve-Beta Cell Interactions in Diabetes
Diabetes is a complex condition that involves multiple factors, including the parasympathetic nerve and beta cells. The dysfunction of these components can have a significant impact on glucose regulation and overall disease progression.
When the parasympathetic nervous system is not functioning properly, it can lead to impaired insulin secretion. Insulin is essential for facilitating the uptake of glucose by cells, allowing them to use it as a source of energy. Without sufficient insulin, glucose remains in the bloodstream, leading to high blood sugar levels. This dysregulation of glucose can have detrimental effects on various organs and tissues in the body.
Conversely, impaired beta cell function can also contribute to abnormal parasympathetic activity. Beta cells play a crucial role in sensing glucose levels and releasing insulin accordingly. When beta cells are not functioning optimally, they may not respond appropriately to changes in blood sugar levels, disrupting the delicate balance between the parasympathetic nerve and beta cells. This dysregulation can further exacerbate glucose dysregulation and contribute to the progression of diabetes.
The Potential for Therapeutic Interventions Targeting the Parasympathetic Nerve and Beta Cells
Recognizing the importance of parasympathetic nerve-beta cell interactions in diabetes, researchers have been exploring potential therapeutic interventions that target these components. By modulating parasympathetic activity or enhancing beta cell function, it may be possible to improve glucose regulation and ultimately manage diabetes more effectively.
One approach to modulating parasympathetic activity is through pharmacological interventions. Certain medications can target the parasympathetic nervous system, either by enhancing its activity or inhibiting its effects. By fine-tuning the parasympathetic response, it may be possible to improve insulin secretion and glucose regulation in individuals with diabetes.
Lifestyle interventions also hold promise in optimizing parasympathetic nerve function and beta cell health. Regular physical activity, a balanced diet, and stress management techniques have been shown to positively influence parasympathetic activity and improve insulin sensitivity. These lifestyle modifications can have a significant impact on glucose regulation and may complement pharmacological approaches in managing diabetes.
Furthermore, innovative approaches aiming to enhance beta cell health and insulin secretion are being explored. Researchers are investigating various strategies, such as gene therapy, stem cell transplantation, and regenerative medicine, to promote the growth and function of beta cells. By improving beta cell health, it may be possible to restore the delicate balance between the parasympathetic nerve and beta cells, leading to improved glucose regulation in individuals with diabetes.
However, it is important to note that further research is needed to validate the efficacy and safety of these approaches. While the potential for therapeutic interventions targeting the parasympathetic nerve and beta cells is promising, it is crucial to ensure that any interventions are evidence-based and tailored to individual needs.
Future Directions in Parasympathetic Nerve and Beta Cell Research
The study of parasympathetic nerve-beta cell interactions is a rapidly evolving field, driven by advancements in technology and a greater understanding of their significance in health and disease. Emerging research aims to uncover the precise molecular mechanisms underlying these interactions, identify novel therapeutic targets, and develop innovative treatment approaches. By unraveling the complex interplay between the parasympathetic nerve and beta cells, researchers hope to develop personalized strategies for managing glucose regulation and improving overall health outcomes.
Emerging Research on Parasympathetic Nerve-Beta Cell Interactions
Recent studies have yielded intriguing insights into the role of parasympathetic nerve-beta cell interactions in various physiological processes beyond glucose regulation. For example, researchers have discovered potential links between these interactions and appetite regulation, gastrointestinal motility, and even mental well-being. These findings open up new avenues for research and have the potential to revolutionize our understanding of the parasympathetic nerve and beta cell interplay.
Potential Innovations in Treatment Approaches
As research in this field advances, there is growing optimism regarding the development of innovative treatment approaches targeting parasympathetic nerve-beta cell interactions. These approaches may involve the use of novel pharmaceutical agents, gene therapies, or even non-invasive neuromodulation techniques. By capitalizing on our evolving understanding of these interactions, researchers strive to improve the management of metabolic disorders and enhance overall health outcomes.
In conclusion, the role of the parasympathetic nerve in beta cell function is a fascinating area of research with profound implications for glucose regulation and overall health. The complex interplay between the parasympathetic nervous system and beta cells underscores the importance of a multidisciplinary approach in unraveling the underlying mechanisms. As our understanding of these interactions deepens, so too does the potential for developing innovative therapeutic interventions that optimize parasympathetic nerve-beta cell communication and improve glucose homeostasis.