Bladder control is a crucial aspect of our daily lives, allowing us to carry out our activities with confidence and comfort. The parasympathetic nerve, a branch of the autonomic nervous system, plays a vital role in regulating bladder function. Understanding the mechanisms and nuances of this complex system is key to developing effective strategies for managing bladder control issues.
Understanding the Parasympathetic Nervous System
The parasympathetic nervous system, often referred to as the “rest and digest” system, works in opposition to the sympathetic nervous system. While the sympathetic system prepares our bodies for action by increasing heart rate and suppressing certain functions, the parasympathetic system promotes relaxation and restoration. Its primary function is to conserve and restore energy by reducing heart rate, constricting blood vessels, and stimulating digestive processes.
When we experience a stressful situation, such as encountering a dangerous animal, the sympathetic nervous system kicks into gear, preparing us for fight or flight. Our heart rate increases, blood vessels constrict, and blood is redirected to our muscles to provide them with the necessary oxygen and nutrients. At the same time, the parasympathetic nervous system takes a backseat, allowing the sympathetic system to take control.
However, once the danger has passed, the parasympathetic system takes over, bringing our bodies back to a state of calm and relaxation. It slows down our heart rate, dilates blood vessels, and activates digestive processes. This allows our bodies to focus on restorative functions, such as repairing tissues, replenishing energy stores, and eliminating waste.
Key Functions of the Parasympathetic Nervous System
The parasympathetic nervous system controls numerous bodily functions, including bladder control. It regulates the contraction and relaxation of the bladder muscles, allowing for efficient urine storage and elimination. This delicate balance is necessary to ensure we can control the timing and frequency of urination.
When the bladder is full, sensory signals are sent to the brain, triggering the parasympathetic system to initiate the relaxation of the bladder muscles. This allows the bladder to expand and accommodate the incoming urine. Simultaneously, the parasympathetic system stimulates the contraction of the bladder’s smooth muscles, pushing the urine towards the urethra for elimination.
In addition to bladder control, the parasympathetic system also plays a vital role in other bodily functions, such as salivation, lacrimation (tear production), and sexual arousal. It is responsible for stimulating the production of saliva, tears, and mucus, which help lubricate and protect various tissues in our body. Furthermore, the parasympathetic system promotes sexual arousal by increasing blood flow to the genital organs and facilitating the release of sexual hormones.
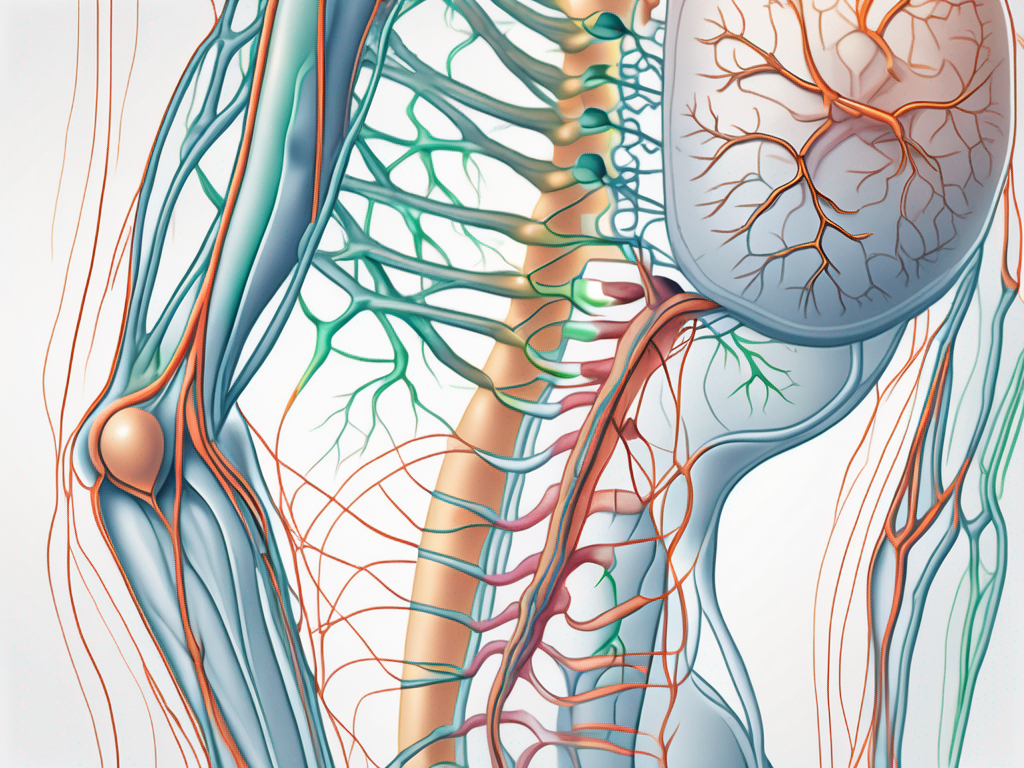
Anatomy of the Parasympathetic Nervous System
The parasympathetic nervous system consists of two main components: cranial and sacral. The cranial component originates from the brainstem and includes cranial nerves that innervate various organs, including the bladder. These cranial nerves, such as the vagus nerve, carry signals from the brain to the target organs, allowing for precise control and coordination of parasympathetic responses.
On the other hand, the sacral component arises from the sacral spinal cord and also plays a crucial role in bladder control. The parasympathetic fibers originating from the sacral region travel through the pelvic nerves and innervate the bladder, as well as the reproductive organs and the lower part of the digestive system. This intricate network of nerves ensures that the parasympathetic system can finely regulate the functions of these organs.
Overall, the parasympathetic nervous system is a vital component of our autonomic nervous system, working in harmony with the sympathetic system to maintain homeostasis and ensure our overall well-being. By understanding its functions and anatomy, we can appreciate the intricate mechanisms that allow our bodies to rest, digest, and maintain optimal bodily functions.
The Parasympathetic Nerve and Bladder Control
Bladder control is a complex interplay between nerve signals, muscle contractions, and conscious control. The parasympathetic nerve, specifically the cranial and sacral components, is heavily involved in this intricate process.
The Neurological Control of the Bladder
In a healthy individual, bladder control begins with the detection of urine accumulation. Nerve signals are sent from the bladder to the brain, notifying us of the need to urinate. This crucial communication is facilitated by the parasympathetic nerve, which acts as the messenger between the bladder and the brain.
Once the brain receives the signal, it initiates a cascade of events to ensure proper bladder function. The parasympathetic nerve communicates with the bladder muscles, triggering their contraction and urging the bladder to empty. This coordinated effort ensures that urine is expelled efficiently and effectively.
Furthermore, the parasympathetic nerve also plays a role in regulating the tone of the bladder muscles. It helps maintain the necessary tension in the bladder wall to prevent leakage and maintain continence. This delicate balance between muscle contraction and relaxation is crucial for maintaining optimal bladder control.
The Impact of the Parasympathetic Nerve on Bladder Function
Disruptions in the parasympathetic nervous system can significantly impair bladder control. Conditions such as nerve damage, spinal cord injuries, or diseases that affect the nerve pathways can lead to dysfunction in this crucial system.
When the parasympathetic nerve is compromised, it can result in various bladder dysfunctions. One common issue is involuntary urine leakage, also known as urinary incontinence. This occurs when the bladder muscles contract uncontrollably, leading to the unintentional release of urine. It can be embarrassing and significantly impact a person’s quality of life.
Another problem that can arise from parasympathetic nerve dysfunction is bladder spasms. These spasms are involuntary contractions of the bladder muscles that can cause sudden and intense urges to urinate. They can be painful and disruptive, making it difficult for individuals to engage in daily activities without frequent interruptions.
In addition to involuntary urine leakage and bladder spasms, dysfunction in the parasympathetic nerve can also result in difficulty initiating or completing urination. This can manifest as a weak urine stream, a feeling of incomplete emptying, or the need to strain during urination. These symptoms can be frustrating and may require medical intervention to restore proper bladder function.
In conclusion, the parasympathetic nerve plays a vital role in bladder control. It acts as the messenger between the bladder and the brain, facilitating the communication necessary for proper urination. Disruptions in this intricate system can lead to various bladder dysfunctions, impacting an individual’s daily life. Understanding the importance of the parasympathetic nerve in bladder control can help in the development of effective treatments and interventions for those experiencing bladder-related issues.
Disorders Related to Parasympathetic Nerve and Bladder Control
Several disorders are closely linked to parasympathetic nerve dysfunction and bladder control issues. Understanding the implications of these disorders is crucial in providing appropriate support and management strategies.
When it comes to the parasympathetic nerve and bladder control, two common disorders that can arise are overactive bladder (OAB) and neurogenic bladder dysfunction.
Overactive Bladder and the Parasympathetic Nerve
Overactive bladder (OAB) is a common condition characterized by an uncontrollable urge to urinate, often accompanied by frequent urination and nocturia. The parasympathetic nerve plays a vital role in both the storage and emptying phases of the bladder, and any dysfunction in this pathway can contribute to OAB symptoms.
When the parasympathetic nerve is not functioning properly, it can lead to an overactive bladder. This means that the bladder muscles contract involuntarily, causing the urge to urinate even when the bladder is not full. This can be quite distressing for individuals experiencing OAB, as it can disrupt daily activities and lead to social embarrassment.
Managing OAB involves a combination of lifestyle modifications, behavioral therapies, and medication. Lifestyle modifications may include avoiding bladder irritants such as caffeine and alcohol, practicing pelvic floor exercises, and maintaining a healthy weight. Behavioral therapies, such as bladder training and scheduled voiding, can help retrain the bladder and improve control. Medications that target the parasympathetic nerve, such as anticholinergics, can also be prescribed to reduce bladder muscle contractions and alleviate OAB symptoms.
Neurogenic Bladder Dysfunction
Neurogenic bladder dysfunction occurs when there is damage or dysfunction in the nerves that control bladder function. This can be due to conditions such as spinal cord injuries, multiple sclerosis, or stroke. The parasympathetic nerve is often affected in these cases, leading to various bladder control problems, including urinary retention, incontinence, or a lack of bladder sensation.
When the parasympathetic nerve is damaged or not functioning properly, it can result in neurogenic bladder dysfunction. Depending on the severity of the nerve damage, individuals may experience different bladder control issues. Some may have difficulty emptying the bladder completely, leading to urinary retention and an increased risk of urinary tract infections. Others may have difficulty holding urine, resulting in urinary incontinence. In some cases, individuals may even lose the sensation of needing to urinate, which can lead to bladder overdistension and potential complications.
Treatment for neurogenic bladder dysfunction focuses on managing symptoms and preventing complications. This may involve techniques such as intermittent catheterization to empty the bladder, medications to relax the bladder muscles or increase bladder contractions, and surgical interventions to improve bladder function. Rehabilitation programs, including pelvic floor exercises and bladder training, may also be recommended to optimize bladder control.
In conclusion, disorders related to parasympathetic nerve dysfunction and bladder control can significantly impact an individual’s quality of life. Whether it is an overactive bladder or neurogenic bladder dysfunction, understanding the underlying mechanisms and implementing appropriate management strategies is essential in providing effective support and improving bladder function.
Treatment and Management of Bladder Control Issues
Effective management of bladder control issues requires a comprehensive approach that addresses the underlying causes and aims to restore optimal function. While professional medical advice should always be sought, there are various treatments and interventions that may be considered in collaboration with a healthcare provider.
Medications Impacting the Parasympathetic Nerve
In certain cases, medications that target the parasympathetic nervous system may be prescribed to manage bladder control issues. These medications work by modulating the nerve signals that regulate bladder contractions and can help in cases of overactive bladder or neurogenic bladder dysfunction. However, it is essential to consult with a healthcare professional to determine the most suitable medication and dosage for individual needs.
When it comes to medications impacting the parasympathetic nerve, there are several options available. One commonly prescribed medication is oxybutynin, which helps relax the bladder muscles and reduce the frequency of involuntary contractions. Another medication that may be considered is tolterodine, which acts similarly to oxybutynin but with potentially fewer side effects. Additionally, mirabegron, a beta-3 adrenergic agonist, can be used to relax the bladder muscles and increase the bladder’s storage capacity.
It is important to note that while these medications can be effective in managing bladder control issues, they may also have side effects. Common side effects include dry mouth, constipation, blurred vision, and dizziness. It is crucial to discuss any concerns or potential side effects with a healthcare professional before starting any medication.
Non-Pharmacological Interventions for Bladder Control
Alongside medication, non-pharmacological approaches can also play a significant role in managing bladder control issues. Strategies such as pelvic floor muscle exercises, bladder training techniques, and lifestyle modifications, including proper hydration and dietary adjustments, may improve bladder function. Consulting with a healthcare provider or seeking the guidance of a pelvic floor physiotherapist can provide personalized guidance on these interventions.
Pelvic floor muscle exercises, also known as Kegel exercises, are designed to strengthen the muscles that support the bladder and control urine flow. These exercises involve contracting and relaxing the pelvic floor muscles, which can help improve bladder control and reduce urinary incontinence. It is important to perform these exercises correctly and consistently for optimal results, and a healthcare professional or pelvic floor physiotherapist can provide guidance on the appropriate technique.
Bladder training techniques involve gradually increasing the time between bathroom visits to train the bladder to hold larger volumes of urine. This approach can be particularly helpful for individuals with an overactive bladder or frequent urination. By gradually extending the time between bathroom breaks, the bladder can learn to stretch and accommodate larger volumes of urine, leading to improved bladder control.
In addition to exercises and training techniques, making certain lifestyle modifications can also contribute to better bladder control. Proper hydration is essential, as both dehydration and excessive fluid intake can negatively impact bladder function. It is recommended to drink an adequate amount of water throughout the day, avoiding excessive caffeine and alcohol consumption, as these substances can irritate the bladder and worsen symptoms.
Dietary adjustments can also play a role in managing bladder control issues. Certain foods and beverages, such as spicy foods, citrus fruits, and carbonated drinks, can irritate the bladder and trigger symptoms. It may be beneficial to identify and avoid these triggers to minimize bladder discomfort and improve control.
Overall, a comprehensive approach to bladder control issues involves a combination of medication, non-pharmacological interventions, and lifestyle modifications. Working closely with a healthcare provider can help determine the most suitable treatment plan tailored to individual needs, ensuring the best possible outcome in managing bladder control issues.
Future Research Directions in Parasympathetic Nerve and Bladder Control
As our understanding of the parasympathetic nerve and bladder control continues to expand, it paves the way for exciting possibilities in research and treatment development. Ongoing studies and emerging technologies offer hope for advancements in managing bladder control issues.
The parasympathetic nerve, also known as the “rest and digest” system, plays a crucial role in maintaining bladder control. This intricate network of nerves communicates with the bladder, signaling when it’s time to empty and coordinating the relaxation of the bladder muscles. Dysfunction in this delicate system can lead to various bladder control issues, impacting the quality of life for affected individuals.
Potential Innovations in Bladder Control Treatment
Researchers are exploring new avenues for improving bladder control treatment. Advancements in neurostimulation techniques, such as sacral neuromodulation and peripheral nerve stimulation, show promise in selectively modulating the nerve signals involved in bladder control. These innovative approaches could potentially offer more targeted and personalized therapies for individuals with bladder control issues.
Furthermore, ongoing research is investigating the potential of gene therapy in treating bladder control disorders. By targeting specific genes involved in the regulation of bladder function, scientists aim to develop novel therapeutic strategies that can restore normal bladder control.
The Future of Neuro-Urology
Neuro-urology, the intersection of neurology and urology, is a rapidly evolving field with a primary focus on understanding and managing bladder control disorders. With continued advancements in neuroscience and technology, we can expect further breakthroughs in diagnosis and treatment options.
One area of interest is the development of non-invasive diagnostic tools that can provide detailed information about the functioning of the parasympathetic nerve and its interaction with the bladder. These tools may include advanced imaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), which can provide valuable insights into the neural pathways involved in bladder control.
In addition to diagnostic advancements, researchers are also exploring the potential of regenerative medicine in restoring bladder function. Stem cell therapy, for example, holds promise in regenerating damaged nerves and muscles in the bladder, potentially offering a long-term solution for individuals with bladder control issues.
Collaborative efforts between researchers, healthcare providers, and patients will undoubtedly shape the future of neuro-urology and, ultimately, improve the lives of individuals affected by bladder control issues. By sharing knowledge, resources, and expertise, the medical community can work together to develop comprehensive and effective treatment strategies.
In conclusion, the parasympathetic nerve plays a crucial role in maintaining bladder control. Dysfunction in this delicate system can lead to various bladder control issues, impacting the quality of life for affected individuals. Seeking professional medical advice is paramount in managing these conditions, as treatment approaches can vary based on the underlying causes and individual needs.
As the field of neuro-urology continues to evolve, ongoing research and technological advancements offer hope for improving diagnosis and treatment options, bringing us closer to a future with more effective strategies for managing bladder control issues. By embracing innovation and collaboration, we can pave the way for a brighter future where individuals with bladder control issues can regain control over their lives and enjoy improved overall well-being.