The bladder parasympathetic nerve plexus is a crucial component of the complex urinary system, playing a vital role in bladder control. As understanding its anatomy, physiology, and related disorders is essential, this comprehensive guide aims to shed light on this often overlooked aspect of our body’s intricate mechanisms.
The Anatomy of the Bladder Parasympathetic Nerve Plexus
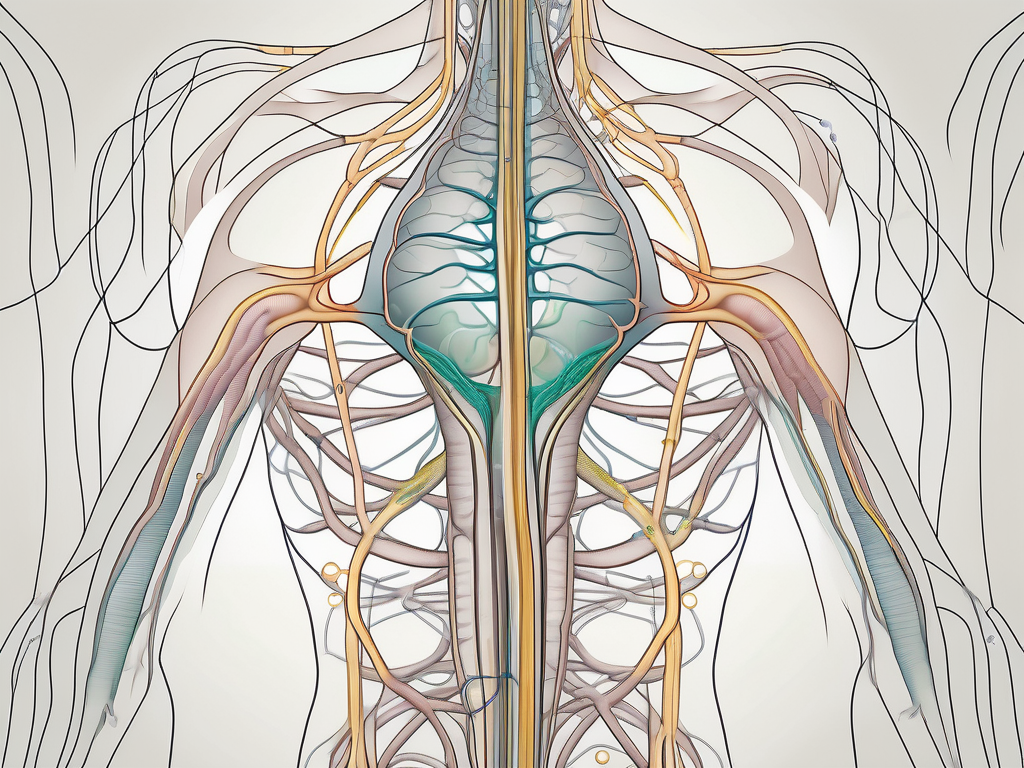
The bladder parasympathetic nerve plexus is a network of nerves located within the lower urinary tract. It works in harmony with other components of the nervous system to regulate bladder function. By communicating with the brain, the bladder parasympathetic nerve plexus enables the coordinated contraction and relaxation of the bladder muscles, allowing us to control the timing and flow of urination.
But what exactly is the bladder parasympathetic nerve plexus and how does it function? Let’s delve deeper into its role and significance in the intricate workings of the urinary system.
It is essential to note that the bladder parasympathetic nerve plexus does not work in isolation. It is influenced by a range of factors, including sensory input from the bladder, signals from the Central Nervous System (CNS), and hormonal regulation. The intricate interplay between these elements ensures the smooth functioning of the urinary system.
The Role of the Parasympathetic Nervous System in Bladder Control
The parasympathetic nervous system, of which the bladder parasympathetic nerve plexus is a part, is responsible for regulating various involuntary bodily functions. Within the realm of bladder control, the parasympathetic nervous system has a significant impact. When the bladder fills with urine, sensory signals are sent to the brain, triggering a parasympathetic response that initiates bladder contractions and relaxes the urinary sphincter, allowing for the expulsion of urine.
This intricate process ensures that we can control the timing and flow of urination, preventing any embarrassing or inconvenient situations. The parasympathetic nervous system acts as a conductor, orchestrating the symphony of bladder function.
Understanding the role of the parasympathetic nervous system in bladder control is crucial in comprehending the mechanisms at play in various bladder disorders, such as overactive bladder and neurogenic bladder. These conditions can disrupt the delicate balance of the parasympathetic nerve plexus, leading to urinary symptoms and a decreased quality of life.
If you are experiencing any urinary symptoms, it is advisable to consult with a healthcare professional who can provide a comprehensive evaluation and guide you towards appropriate management strategies.
Key Components of the Bladder Parasympathetic Nerve Plexus
The bladder parasympathetic nerve plexus consists of several essential components that work in unison to regulate bladder function. The main players include the pelvic nerves, the sacral spinal cord, and the ganglia located in the pelvic region. These components form a complex network of communication pathways that ensure the smooth coordination of bladder contractions and relaxation.
The pelvic nerves carry signals from the sacral spinal cord to the bladder, providing the necessary communication between the brain and the urinary system. Without these nerves, the brain would not be able to regulate bladder function effectively.
Within the ganglia, various neurotransmitters and receptors are present, facilitating the transmission of signals and modulating bladder function. These neurotransmitters, such as acetylcholine, play a crucial role in the communication between nerve cells and ensure the proper functioning of the parasympathetic nerve plexus.
Dysfunction or damage to any of these components can lead to bladder parasympathetic nerve plexus disorders, affecting urinary control and overall quality of life. It is important to recognize the significance of each component and the role they play in maintaining a healthy bladder.
In conclusion, the bladder parasympathetic nerve plexus is a vital component of the urinary system, working in harmony with other elements to regulate bladder function. Its role in bladder control and the interplay between various factors highlight the complexity of the urinary system. By understanding the anatomy and function of the bladder parasympathetic nerve plexus, we can gain insights into the mechanisms underlying bladder disorders and work towards effective management strategies.
The Physiology of the Bladder Parasympathetic Nerve Plexus
Understanding the physiology of the bladder parasympathetic nerve plexus is crucial for comprehending the process of urination and the interplay between the nervous and urinary systems.
The bladder parasympathetic nerve plexus, a complex network of nerves, plays a vital role in regulating the function of the bladder. This intricate system ensures that the bladder can efficiently store and eliminate urine, maintaining proper urinary control.
The Process of Urination: A Closer Look
Urination is a finely coordinated process that involves several steps, regulated by the bladder parasympathetic nerve plexus. As the bladder fills with urine, sensory signals are transmitted to the brain, signaling the need for voiding. These signals are processed and interpreted by the brain, which then initiates the appropriate response.
In response to the brain’s signals, the parasympathetic nervous system is activated. This activation triggers a series of events that result in the contraction of the bladder muscle and the relaxation of the urinary sphincter. The bladder muscle contracts, exerting pressure on the urine within, while the urinary sphincter relaxes, allowing urine to flow out of the bladder and into the urethra.
These coordinated actions allow for the expulsion of urine from the body, providing relief and maintaining the proper functioning of the urinary system. Once the bladder is emptied, the parasympathetic activity subsides, and the bladder returns to a relaxed state, ready for the next filling cycle.
The Interplay between the Nervous System and the Urinary System
The nervous system and the urinary system work synergistically to ensure proper bladder control. The bladder parasympathetic nerve plexus receives signals from the brain, integrating them with sensory input from the bladder to initiate appropriate bladder contractions and sphincter relaxation.
Furthermore, the nervous system communicates with the urinary system through hormonal regulation, particularly involving antidiuretic hormone (ADH) and aldosterone. These hormones influence the body’s fluid balance and subsequently impact bladder function. ADH, also known as vasopressin, regulates the amount of water reabsorbed by the kidneys, affecting the volume of urine produced. Aldosterone, on the other hand, regulates the reabsorption of sodium and water in the kidneys, further influencing urine production and bladder function.
Understanding this intricate interplay is essential for a comprehensive understanding of bladder parasympathetic nerve plexus function. It highlights the complex nature of the human body and the intricate mechanisms that ensure proper urinary control.
Disorders Related to the Bladder Parasympathetic Nerve Plexus
Disorders related to the bladder parasympathetic nerve plexus can significantly impact an individual’s urinary control and quality of life. The bladder parasympathetic nerve plexus plays a crucial role in the regulation of bladder function, and any dysfunction in this system can lead to various conditions that affect the bladder’s ability to store and empty urine effectively. Two common conditions that deserve attention are overactive bladder and neurogenic bladder.
Overactive Bladder and the Parasympathetic Nervous System
An overactive bladder is characterized by a sudden and uncontrollable urge to urinate, often accompanied by increased daytime and nighttime frequency. This condition can be disruptive and distressing, impacting an individual’s daily activities and overall well-being. While the exact causes can vary, dysfunction in the parasympathetic nervous system, including the bladder parasympathetic nerve plexus, is believed to contribute to this condition.
The parasympathetic nervous system is responsible for promoting bladder relaxation and filling. When this system malfunctions, it can lead to an overactive bladder. The bladder parasympathetic nerve plexus, which is a network of nerves that innervates the bladder, plays a crucial role in coordinating the relaxation of the bladder muscles and the contraction of the bladder neck during urination. Any disruption in this coordination can result in the symptoms associated with an overactive bladder.
Management strategies for overactive bladder range from behavioral modifications and pelvic floor exercises to medications that target the parasympathetic system. Behavioral modifications may include bladder training techniques, such as scheduled voiding and fluid management, to regain control over bladder function. Pelvic floor exercises, also known as Kegel exercises, can help strengthen the muscles that support the bladder and improve urinary control.
In cases where conservative measures are not sufficient, medications that target the parasympathetic system may be prescribed. These medications work by blocking the signals that trigger bladder contractions, helping to reduce the frequency and urgency associated with an overactive bladder. Consulting with a healthcare professional can help determine the most appropriate approach for each individual, taking into consideration their specific symptoms, medical history, and lifestyle.
Neurogenic Bladder: Causes and Implications
Neurogenic bladder refers to a dysfunction of the bladder due to nerve damage or neurological disorders. This condition can lead to bladder paralysis, causing challenges with bladder emptying and retention. The parasympathetic system, including the bladder parasympathetic nerve plexus, is heavily involved in the regulation of neurogenic bladder.
There are various causes of neurogenic bladder, including spinal cord injuries, multiple sclerosis, Parkinson’s disease, and stroke. In these conditions, the nerves that control bladder function may be damaged or disrupted, leading to impaired communication between the brain, spinal cord, and bladder. As a result, the bladder may not receive the appropriate signals to contract or relax, leading to difficulties in emptying or retaining urine.
Treatment for neurogenic bladder may involve medications, catheterization, or surgical interventions, depending on the underlying cause and severity of the condition. Medications can help improve bladder function by targeting the parasympathetic system and promoting coordination between the bladder muscles and the bladder parasympathetic nerve plexus. Catheterization, both intermittent and indwelling, may be necessary to ensure proper bladder emptying and prevent urinary retention.
In some cases, surgical interventions may be required to address the underlying cause of neurogenic bladder. For example, if the condition is caused by a spinal cord injury, surgery may be performed to stabilize the spine and relieve pressure on the nerves. A consultation with a healthcare professional who specializes in neurogenic bladder management is crucial to develop an individualized treatment plan that addresses the specific needs and challenges of each patient.
Treatment and Management of Bladder Parasympathetic Nerve Plexus Disorders
Treatment and management options for bladder parasympathetic nerve plexus disorders aim to address the underlying causes, alleviate symptoms, and improve overall bladder control. These strategies can range from medical interventions to surgical procedures. It is important to note that the specific treatment plan will depend on the individual’s condition, severity of symptoms, and medical history.
One commonly used approach in the treatment of bladder parasympathetic nerve plexus disorders is the use of medications. Medications, such as anticholinergics or beta-3 agonists, are often prescribed to target the parasympathetic system and modulate bladder function. Anticholinergics work by blocking the action of acetylcholine, a neurotransmitter that stimulates bladder contractions. By doing so, these medications help reduce bladder overactivity and improve urinary control. On the other hand, beta-3 agonists work by activating specific receptors in the bladder, leading to relaxation of the bladder muscle and increased bladder capacity. However, it is essential to consult with a healthcare professional before starting any medication to ensure proper assessment and guidance.
In addition to medications, other non-surgical interventions may be recommended to manage bladder parasympathetic nerve plexus disorders. These can include lifestyle modifications, such as bladder training exercises, pelvic floor muscle exercises, and dietary changes. Bladder training exercises involve gradually increasing the time between bathroom visits to improve bladder capacity and control. Pelvic floor muscle exercises, also known as Kegel exercises, aim to strengthen the muscles that support the bladder and control urination. Dietary changes may involve avoiding certain foods and beverages that can irritate the bladder, such as caffeine, alcohol, and spicy foods.
In cases where conservative management approaches do not provide sufficient relief, surgical interventions may be considered. These procedures aim to address the underlying cause of the bladder parasympathetic nerve plexus disorder, restore proper bladder function, and improve urinary control. One surgical option is the implantation of a sacral nerve stimulator, which involves the placement of a small device near the sacral nerves to provide electrical stimulation. This stimulation helps regulate bladder function and can significantly reduce symptoms. Another surgical procedure is bladder augmentation, which involves increasing the size of the bladder by using a segment of the patient’s intestine. This procedure can improve bladder capacity and control, but it is typically reserved for severe cases and carefully evaluated on an individual basis.
It is important to note that the decision to undergo surgery should be made in consultation with a healthcare professional, considering individual circumstances and potential risks and benefits. Surgical interventions carry their own set of risks, including infection, bleeding, and complications related to anesthesia. Therefore, a thorough evaluation of the patient’s overall health and the severity of the bladder parasympathetic nerve plexus disorder is crucial in determining the most appropriate treatment approach.
Future Research Directions in Bladder Parasympathetic Nerve Plexus
The field of bladder parasympathetic nerve plexus research is continuously evolving, with ongoing studies exploring innovative approaches to bladder control and management.
Bladder parasympathetic nerve plexus disorders affect millions of people worldwide, causing a range of symptoms such as urinary incontinence, overactive bladder, and urinary retention. These conditions significantly impact the quality of life for affected individuals, highlighting the importance of continued research in this field.
Innovations in Bladder Control: A Glimpse into the Future
Advancements in technology and research hold promising possibilities for improving bladder control. From neuromodulation techniques to the development of targeted therapies, researchers are exploring novel interventions that could revolutionize the field of bladder parasympathetic nerve plexus disorders.
Neuromodulation techniques, such as sacral nerve stimulation, involve the use of electrical impulses to modulate the activity of the bladder parasympathetic nerve plexus. These techniques have shown promising results in managing overactive bladder and urinary incontinence, providing hope for individuals seeking alternative treatment options.
Additionally, researchers are investigating the potential of biofeedback therapy in improving bladder control. This therapy involves training individuals to become aware of their bladder function and learn techniques to enhance control. Through the use of sensors and visual or auditory cues, biofeedback therapy aims to empower individuals to regain control over their bladder function.
The Potential of Stem Cell Therapy in Treating Bladder Disorders
Stem cell therapy has emerged as a potential avenue for treating various conditions, including bladder disorders. Researchers are investigating the potential of stem cells in regenerating damaged bladder tissues and restoring proper bladder function.
By harnessing the regenerative capabilities of stem cells, scientists aim to develop innovative therapies that can repair and rejuvenate the bladder parasympathetic nerve plexus. This approach holds great promise for individuals with bladder disorders, offering the potential for long-lasting and effective treatment options.
However, it is important to note that stem cell therapy for bladder disorders is still in the experimental stages. Further research and clinical trials are necessary to fully understand the safety, efficacy, and long-term outcomes of this treatment approach.
In conclusion, understanding the intricate workings of the bladder parasympathetic nerve plexus is essential for comprehending bladder control and related disorders. While this comprehensive guide provides valuable insights, it is crucial to consult with a healthcare professional for a thorough evaluation and personalized management strategies.
As research in this field progresses, new opportunities for improving bladder function and quality of life may arise, promising hope for individuals affected by bladder parasympathetic nerve plexus disorders. Continued collaboration between researchers, clinicians, and patients will be instrumental in driving forward the development of innovative therapies and interventions.