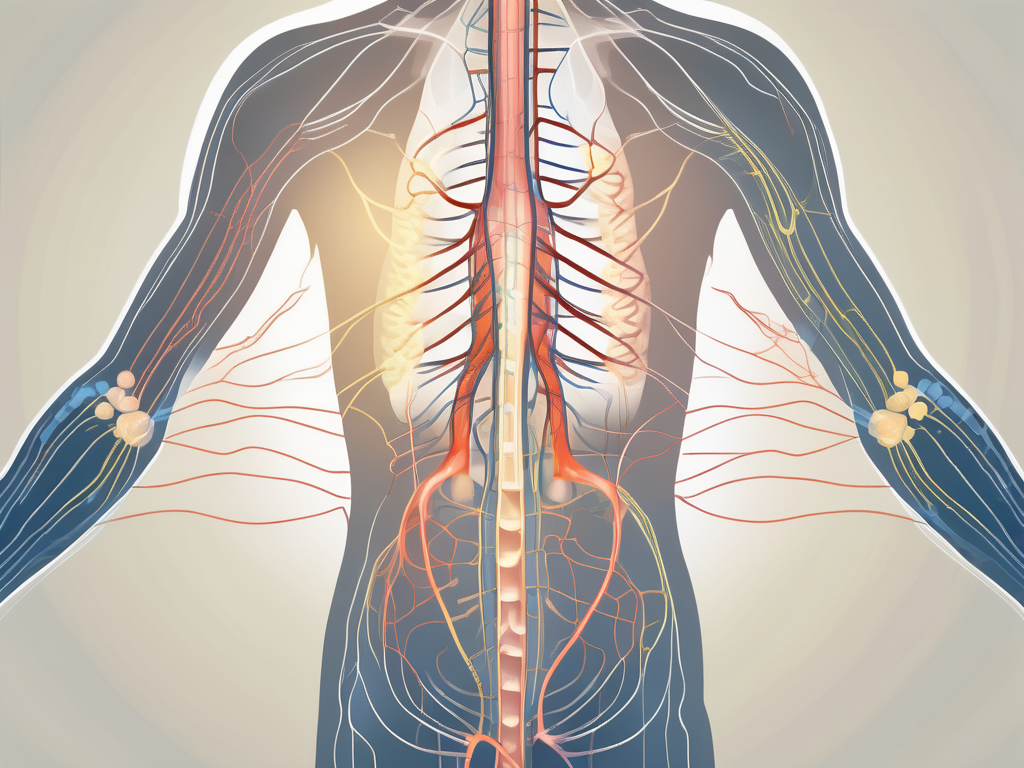
The parasympathetic nervous system plays a crucial role in regulating the functions of the abdominal viscera. Understanding how this intricate network operates is fundamental to comprehending the complex dynamics of the abdominal region. In this comprehensive guide, we will delve into the anatomy, functions, and disorders of the parasympathetic nerve to abdominal viscera, providing you with a detailed understanding of this vital system.
Introduction to the Parasympathetic Nervous System
The parasympathetic nervous system is one of the divisions of the autonomic nervous system. It primarily works to maintain homeostasis by promoting rest, digestion, and relaxation. This branch of the nervous system counterbalances the sympathetic nervous system, which activates the body’s fight-or-flight response. Through its intricate network of nerves, the parasympathetic system influences various organs and their functions, including those in the abdominal region.
The parasympathetic nervous system plays a crucial role in the overall well-being of the body. It is responsible for regulating numerous bodily functions, ensuring that they operate smoothly and efficiently. By understanding the intricacies of this system, we can gain insight into how our bodies maintain equilibrium and respond to different situations.
The Role of the Parasympathetic Nervous System
The primary role of the parasympathetic nervous system is to regulate visceral functions and maintain the body’s internal balance. It accomplishes this by stimulating the secretion of digestive enzymes and increasing blood flow to the abdominal organs. This increased blood flow ensures that the organs receive an adequate supply of oxygen and nutrients, promoting optimal functioning.
Moreover, the parasympathetic system helps in the elimination of waste through the activation of intestinal peristalsis and the release of bile in the liver. These processes aid in the efficient breakdown and absorption of nutrients, ensuring that the body receives the necessary fuel to carry out its daily activities.
Additionally, the parasympathetic nervous system plays a vital role in promoting relaxation and reducing stress. When activated, it slows down the heart rate, lowers blood pressure, and promotes a sense of calmness. This allows the body to conserve energy and focus on essential restorative processes, such as tissue repair and growth.
Components of the Parasympathetic Nervous System
The parasympathetic nervous system consists of two main components: cranial nerves and sacral nerves. The cranial nerves originate in the brain and directly innervate various organs in the head and neck region, while the sacral nerves arise from the sacral region of the spinal cord and innervate the pelvic organs.
These components work in harmony to regulate abdominal visceral functions. The cranial nerves, including the vagus nerve, play a crucial role in controlling digestion and other vital processes. They stimulate the secretion of digestive juices, such as saliva and gastric acid, which aid in the breakdown of food. Additionally, they regulate the contraction and relaxation of smooth muscles in the gastrointestinal tract, ensuring efficient movement of food through the digestive system.
The sacral nerves, on the other hand, are responsible for innervating the pelvic organs, including the bladder and reproductive organs. They control the release of urine and facilitate sexual arousal and reproduction. By coordinating the activities of these organs, the parasympathetic system ensures their proper functioning and contributes to overall abdominal health.
In conclusion, the parasympathetic nervous system is a vital component of the autonomic nervous system. It plays a crucial role in maintaining homeostasis, promoting rest and relaxation, and regulating abdominal visceral functions. By understanding the intricate workings of this system, we can appreciate the complexity of our bodies and the remarkable balance they strive to achieve.
Anatomy of the Parasympathetic Nerve to Abdominal Viscera
The anatomy of the parasympathetic nerve to abdominal viscera is a fascinating subject that provides insights into the intricate pathways and distribution of these vital nerves.
The parasympathetic nerve fibers that innervate the abdominal viscera originate from specific regions within the central nervous system. The cranial nerves associated with this system include the vagus nerve (cranial nerve X), while the sacral nerves contribute through the pelvic splanchnic nerves. These nerves travel along specific pathways, synapse at ganglia, and then continue to innervate various abdominal organs.
Understanding the origin and pathway of the parasympathetic nerve to abdominal viscera is crucial in comprehending the complex network that regulates the functions of these organs. The vagus nerve, originating in the brainstem, plays a significant role in this intricate system. It extends its branches to reach the stomach, liver, pancreas, and intestines, among other abdominal organs.
Once the parasympathetic nerves reach the abdominal region, they branch out extensively to innervate the different organs. The vagus nerve, for example, branches into the gastric, hepatic, pancreatic, and intestinal branches, among others. These branches form an intricate network, allowing for the precise regulation of each organ’s functions.
The gastric branches of the vagus nerve are responsible for regulating the secretion of gastric acid and enzymes, as well as the motility of the stomach. These branches ensure the proper digestion and absorption of nutrients, playing a crucial role in maintaining overall gastrointestinal health.
The hepatic branches of the vagus nerve provide parasympathetic innervation to the liver, influencing various hepatic functions. These include the regulation of glycogen storage, bile production, and the metabolism of lipids, proteins, and carbohydrates. The intricate interplay between the parasympathetic nervous system and the liver is essential for maintaining metabolic homeostasis.
The pancreatic branches of the vagus nerve play a vital role in regulating pancreatic secretion. These branches stimulate the release of digestive enzymes, such as amylase, lipase, and protease, which are crucial for the breakdown of carbohydrates, fats, and proteins. Additionally, they also influence the release of insulin and glucagon, hormones involved in glucose regulation.
The intestinal branches of the vagus nerve innervate the small and large intestines, contributing to the regulation of intestinal motility and absorption. These branches ensure the proper movement of food through the intestines, allowing for efficient nutrient absorption and waste elimination.
The intricate network formed by the parasympathetic nerve branches to the abdominal viscera highlights the complexity and precision of the human body. The coordination and regulation of various organ functions through these nerves are essential for maintaining overall health and well-being.
Functions of the Parasympathetic Nerve to Abdominal Viscera
Understanding the functions of the parasympathetic nerve to the abdominal viscera is crucial to grasp its role in maintaining the overall health and well-being of individuals. The parasympathetic nervous system, often referred to as the “rest and digest” system, plays a significant role in regulating various processes within the abdominal cavity.
Role in Digestion
The parasympathetic nervous system has a significant impact on digestion. By stimulating the release of digestive enzymes and increasing blood flow to the abdominal organs, it facilitates the breakdown and absorption of nutrients. This process is essential for maintaining proper nutrition and overall digestive health.
When food enters the stomach, the parasympathetic nerve signals the release of gastric juices, including hydrochloric acid and digestive enzymes such as pepsin. These enzymes help break down proteins into smaller molecules that can be easily absorbed by the intestines. Additionally, the parasympathetic nerve stimulates the secretion of pancreatic enzymes, which further aid in the digestion of carbohydrates, fats, and proteins.
Furthermore, the parasympathetic nerve promotes the contraction of smooth muscles in the gastrointestinal tract, facilitating the movement of food through the digestive system. This peristaltic movement ensures that food is properly mixed with digestive enzymes and progresses smoothly from the stomach to the small intestine and eventually to the large intestine.
Impact on Blood Flow
The parasympathetic nerve to abdominal viscera also plays a vital role in regulating blood flow to the abdominal organs. By influencing the diameter of blood vessels, it helps to ensure that vital organs receive an adequate supply of oxygen and nutrients. This involvement in blood flow regulation contributes to the optimal functioning of the abdominal viscera.
When the parasympathetic nerve is activated, it causes the blood vessels supplying the abdominal organs to dilate. This dilation increases blood flow, delivering oxygen and nutrients to the organs, and removing waste products. Adequate blood flow is essential for the proper functioning of organs such as the liver, spleen, and intestines, as it ensures a constant supply of nutrients and oxygen for their metabolic activities.
Regulation of Organ Functions
In addition to digestion and blood flow regulation, the parasympathetic nervous system also influences the functions of specific organs in the abdominal cavity. It aids in bladder emptying, stimulates gallbladder contraction for bile release, and promotes proper bowel movements. Through its intricate control over organ functions, the parasympathetic nerve ensures the smooth operation of the abdominal viscera.
When it comes to bladder emptying, the parasympathetic nerve signals the detrusor muscle in the bladder wall to contract, leading to the expulsion of urine. This process is essential for maintaining urinary continence and preventing bladder-related complications.
The parasympathetic nerve also plays a crucial role in the release of bile from the gallbladder. Upon activation, it stimulates the contraction of the gallbladder, causing the release of bile into the small intestine. Bile is essential for the digestion and absorption of fats, as it helps emulsify dietary fats, making them easier to break down and absorb.
Moreover, the parasympathetic nerve promotes proper bowel movements by stimulating the contraction of smooth muscles in the intestines. This peristaltic movement helps propel fecal matter through the digestive tract, ensuring regular bowel movements and preventing constipation.
In conclusion, the parasympathetic nerve to abdominal viscera plays a crucial role in maintaining the overall health and functioning of the abdominal organs. Its involvement in digestion, blood flow regulation, and organ function control ensures proper nutrient absorption, optimal oxygen and nutrient supply, and the smooth operation of the abdominal viscera. Understanding the functions of this nerve is essential for comprehending the intricate mechanisms underlying abdominal health.
Disorders Related to the Parasympathetic Nerve to Abdominal Viscera
In some instances, the parasympathetic nervous system may experience dysfunction, leading to various disorders that affect the abdominal viscera. Recognizing the symptoms, undergoing appropriate diagnostic procedures, and seeking timely treatment are vital in managing these conditions.
The parasympathetic nervous system plays a crucial role in regulating the functions of the abdominal viscera, including the stomach, intestines, liver, gallbladder, and pancreas. When this system malfunctions, it can result in a range of disorders that disrupt the normal functioning of these organs.
One common disorder related to the parasympathetic nerve to abdominal viscera is gastroesophageal reflux disease (GERD). This condition occurs when the lower esophageal sphincter, which normally prevents stomach acid from flowing back into the esophagus, becomes weak or relaxes inappropriately. As a result, individuals with GERD may experience persistent abdominal pain, heartburn, regurgitation, and difficulty swallowing.
Another disorder that can arise from parasympathetic nerve dysfunction is irritable bowel syndrome (IBS). This chronic condition affects the large intestine and is characterized by abdominal pain, bloating, and alterations in bowel movements. Individuals with IBS may experience diarrhea, constipation, or a combination of both.
Common Symptoms and Signs
Disorders related to the parasympathetic nerve to abdominal viscera can manifest in a variety of symptoms and signs. These may include persistent abdominal pain, alterations in bowel movements, urinary disturbances, and abnormal digestive function. However, it is essential to note that such symptoms can also be indicative of other medical conditions, highlighting the importance of consulting with a healthcare professional for accurate diagnosis.
In addition to the symptoms mentioned above, individuals with parasympathetic nerve dysfunction may also experience changes in their urinary function. The parasympathetic nerves play a role in controlling the bladder and urinary sphincters. Dysfunction in these nerves can lead to urinary incontinence, frequent urination, or difficulty emptying the bladder completely.
Furthermore, abnormal digestive function is another common symptom of disorders related to the parasympathetic nerve to abdominal viscera. This can manifest as difficulties in digesting certain foods, excessive gas production, or changes in appetite.
Diagnostic Procedures
When investigating disorders related to the parasympathetic nerve to abdominal viscera, healthcare providers may employ various diagnostic procedures. These may include medical history taking, physical examinations, blood tests, imaging studies, and specialized tests to assess autonomic nerve function. The aim of these procedures is to identify the underlying cause of the symptoms and determine an appropriate treatment plan.
During a medical history taking, the healthcare provider will inquire about the individual’s symptoms, their duration, and any factors that may exacerbate or alleviate them. This information can provide valuable insights into the possible causes of the parasympathetic nerve dysfunction.
Physical examinations may involve palpating the abdomen to check for tenderness or abnormal masses. The healthcare provider may also perform a rectal examination to assess the tone of the anal sphincter and evaluate the condition of the rectum and lower part of the colon.
Blood tests can help identify any abnormalities in liver function, pancreatic enzymes, or inflammatory markers that may indicate an underlying condition affecting the abdominal viscera.
Imaging studies, such as ultrasound, CT scan, or MRI, may be used to visualize the abdominal organs and detect any structural abnormalities or signs of inflammation.
Specialized tests to assess autonomic nerve function can provide valuable information about the integrity of the parasympathetic nervous system. These tests may include heart rate variability analysis, sudomotor testing, or gastrointestinal motility studies.
Treatment and Management Options
The treatment and management of disorders related to the parasympathetic nerve to abdominal viscera depend on the specific condition and its severity. Management may involve lifestyle modifications, dietary changes, stress reduction techniques, medications, or surgical interventions. It is crucial for individuals experiencing such conditions to work closely with their healthcare providers to develop a personalized treatment plan that addresses their specific needs.
Lifestyle modifications can play a significant role in managing parasympathetic nerve dysfunction. This may include adopting stress-reduction techniques, such as meditation or yoga, to help alleviate symptoms. Regular exercise and maintaining a healthy weight can also contribute to overall well-being and improve digestive function.
Dietary changes may be recommended to individuals with disorders related to the parasympathetic nerve to abdominal viscera. This may involve avoiding trigger foods that worsen symptoms, such as spicy or fatty foods in the case of GERD. Increasing fiber intake and staying hydrated can also help regulate bowel movements and alleviate symptoms of IBS.
In some cases, medications may be prescribed to manage symptoms or address underlying causes. For example, proton pump inhibitors or H2 blockers may be prescribed to reduce stomach acid production in individuals with GERD. Antispasmodic medications or laxatives may be prescribed to individuals with IBS to alleviate abdominal pain or regulate bowel movements.
In more severe cases, surgical interventions may be necessary to correct structural abnormalities or alleviate symptoms that do not respond to conservative treatments. These procedures may involve repairing a weakened lower esophageal sphincter or removing abnormal growths in the intestines.
Overall, the management of disorders related to the parasympathetic nerve to abdominal viscera requires a comprehensive approach that takes into account the individual’s specific symptoms, medical history, and lifestyle factors. By working closely with healthcare providers, individuals can develop an effective treatment plan that aims to improve their quality of life and alleviate the symptoms associated with these disorders.
The Future of Parasympathetic Nerve Research
As medical knowledge continues to expand, researchers are constantly exploring new frontiers in parasympathetic nerve research. This ongoing investigation holds the potential to provide insights into novel techniques and technologies with far-reaching implications.
Emerging Techniques and Technologies
Advancements in medical technology, including neuroimaging and nerve stimulation techniques, are enabling researchers to gain a deeper understanding of the parasympathetic nerve to abdominal viscera. These techniques allow for non-invasive examination of nerve pathways and function, contributing to the development of innovative diagnostic and therapeutic approaches.
Potential Implications for Medical Practice
Research findings related to the parasympathetic nerve system may have significant implications for medical practice. They may lead to the development of targeted therapies for specific disorders, improved diagnostic accuracy, and the enhancement of overall patient care. As our understanding of the parasympathetic nerve to abdominal viscera continues to evolve, these advancements may revolutionize the field of abdominal medicine.
Conclusion
In conclusion, understanding the parasympathetic nerve to abdominal viscera is crucial in comprehending the intricate workings of the body’s digestive and regulatory systems. By gaining insights into the anatomy, functions, and disorders associated with this network, individuals can better appreciate the complexities underlying their abdominal health. It is important always to consult with healthcare professionals to ensure accurate diagnosis and appropriate management of any abdominal health concerns.