The field of medicine is constantly evolving, and one area that has garnered much attention is the use of parasympathetic nerve blockers. These medications play a crucial role in managing various health conditions by modulating the activity of the parasympathetic nervous system. In this comprehensive guide, we will delve into the intricacies of parasympathetic nerve blockers, exploring their mechanism of action, clinical applications, potential side effects, and future perspectives in research.
An Overview of the Nervous System
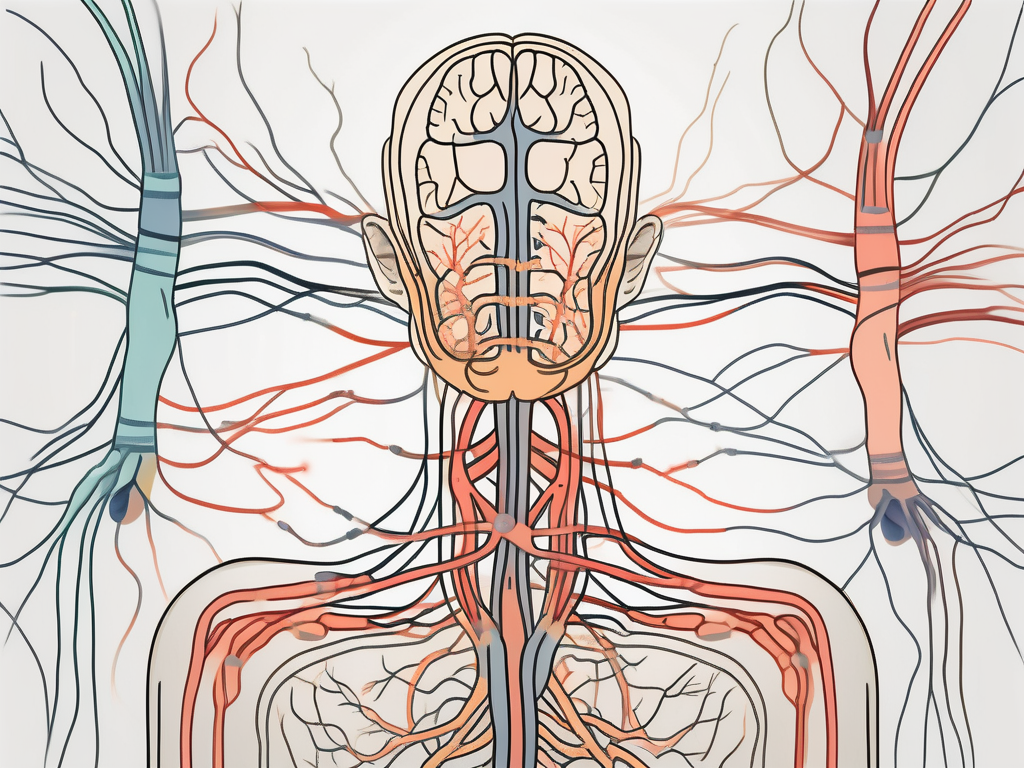
Before diving deep into the world of parasympathetic nerve blockers, it is essential to understand the basics of the nervous system. The nervous system is a complex network of cells that enables communication between different parts of the body, allowing for coordinated responses and maintaining homeostasis.
It consists of two main components: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS comprises the brain and spinal cord, while the PNS encompasses all the nerves outside of the CNS, including the parasympathetic and sympathetic divisions.
The central nervous system, which includes the brain and spinal cord, is like the command center of the body. It receives and processes information from the senses, initiates actions, and coordinates the activities of all the other parts of the body. The brain, with its billions of neurons, is responsible for our thoughts, emotions, memories, and behaviors. The spinal cord, on the other hand, acts as a relay station, transmitting signals between the brain and the rest of the body.
Meanwhile, the peripheral nervous system is like a vast network of highways that connects the CNS to the rest of the body. It consists of nerves that carry information to and from the CNS. These nerves can be further divided into two divisions: the somatic nervous system and the autonomic nervous system.
The somatic nervous system controls voluntary movements and transmits sensory information to the CNS. It allows us to consciously move our muscles, feel sensations like touch and pain, and perceive the world around us.
The autonomic nervous system, on the other hand, controls involuntary actions that occur without conscious thought, such as heart rate, digestion, and breathing. It can be further divided into two branches: the parasympathetic nervous system and the sympathetic nervous system.
The Parasympathetic Nervous System
The parasympathetic division of the PNS is responsible for regulating bodily functions during periods of relaxation and decreased physical activity. It helps conserve energy and facilitates restorative processes by lowering heart rate, promoting digestion, and constricting certain blood vessels. Its influence is most prominent in non-stressful situations, allowing the body to conserve and replenish its resources.
When the parasympathetic nervous system is activated, it promotes a state of calm and relaxation. It allows us to rest and digest, ensuring that our bodies can focus on essential processes like digestion, absorption of nutrients, and elimination of waste. This division of the PNS helps maintain homeostasis by counteracting the effects of the sympathetic nervous system.
The Sympathetic Nervous System
On the other hand, the sympathetic division of the PNS is often referred to as the “fight or flight” system. It prepares the body for action by increasing heart rate, dilating blood vessels, and activating sweat glands. This response is crucial when facing stressful situations or threats, enabling the body to respond quickly and effectively.
When the sympathetic nervous system is activated, it triggers a cascade of physiological changes that prepare the body for action. The heart rate increases, pumping more oxygen-rich blood to the muscles, while blood vessels dilate to allow for increased blood flow. This division of the PNS also causes the release of stress hormones like adrenaline, which heightens alertness and enhances physical performance.
In addition to its role in the fight or flight response, the sympathetic nervous system also plays a role in regulating various bodily functions, such as body temperature, blood pressure, and metabolism. It works in harmony with the parasympathetic nervous system to maintain a delicate balance in the body.
The Science Behind Parasympathetic Nerve Blockers
Parasympathetic nerve blockers primarily target the parasympathetic division of the peripheral nervous system (PNS). By blocking the action of specific neurotransmitters, such as acetylcholine, these medications can modulate the activity of the parasympathetic system in a controlled manner. This modulation can have significant therapeutic benefits in various clinical scenarios, ranging from the treatment of overactive bladder to facilitating muscle relaxation during surgical procedures.
The parasympathetic division of the PNS is responsible for regulating various bodily functions, including digestion, urination, and resting heart rate. It works in opposition to the sympathetic division, which is responsible for the “fight or flight” response. By selectively blocking the parasympathetic system, nerve blockers can help restore balance and alleviate symptoms associated with overactivity or dysfunction.
Mechanism of Action
Parasympathetic nerve blockers exert their effects by binding to specific receptors on target cells or nerve endings, inhibiting the release or blocking the action of acetylcholine. Acetylcholine is a neurotransmitter that plays a crucial role in transmitting signals within the parasympathetic system. By interfering with its function, nerve blockers disrupt the normal regulatory actions of the parasympathetic system, leading to the desired pharmacological effects.
These medications can act on various types of receptors, including muscarinic and nicotinic receptors. Muscarinic receptors are found in smooth muscle, glands, and the heart, while nicotinic receptors are found at the neuromuscular junction. By selectively blocking these receptors, nerve blockers can modulate the activity of different organs and tissues, depending on their specific pharmacological properties.
Types of Parasympathetic Nerve Blockers
Several classes of medications act as parasympathetic nerve blockers, each with its own unique pharmacological profile and clinical indications. Examples include anticholinergic drugs, such as atropine and scopolamine. Atropine is frequently used to treat conditions like overactive bladder, where it helps relax the bladder muscles and reduce urinary urgency. Scopolamine, on the other hand, is commonly used to prevent motion sickness by blocking the action of acetylcholine in the vestibular system.
Neuromuscular blocking agents, such as succinylcholine, also act as parasympathetic nerve blockers. These medications are used in surgical procedures to facilitate muscle relaxation, allowing for easier intubation and surgical access. By blocking the transmission of signals from nerves to muscles, neuromuscular blockers temporarily paralyze specific muscle groups, enabling surgeons to perform procedures more effectively.
It is essential to note that the use of parasympathetic nerve blockers should always be under the supervision of a qualified healthcare professional. These medications require careful assessment and individualized treatment plans based on the patient’s unique medical history and current condition. The dosage and duration of treatment may vary depending on the specific indication and the patient’s response to therapy. Regular monitoring and follow-up are necessary to ensure optimal outcomes and minimize potential side effects.
Clinical Applications of Parasympathetic Nerve Blockers
The clinical utility of parasympathetic nerve blockers extends to various medical specialties, making them valuable tools in the management of numerous conditions.
Parasympathetic nerve blockers, also known as anticholinergics, are medications that inhibit the action of the parasympathetic nervous system. This branch of the autonomic nervous system is responsible for regulating bodily functions such as digestion, salivation, and urination. By blocking the parasympathetic nerves, these medications can have a wide range of effects on the body.
Use in Surgical Procedures
During surgery, parasympathetic nerve blockers can be utilized to achieve specific goals, such as minimizing secretions, inducing muscle relaxation, or preventing unwanted reflexes. These medications aid in optimizing patient comfort and facilitating safe and efficient surgical procedures. However, the precise choice and administration of these drugs should always be determined by the anesthesiologist or attending physician to ensure optimal outcomes.
For example, in ophthalmic surgery, parasympathetic nerve blockers like atropine or tropicamide can be used to dilate the pupil, allowing for better visualization of the surgical field. This is particularly important in procedures such as cataract surgery or retinal detachment repair.
In urological surgeries, parasympathetic nerve blockers like oxybutynin or tolterodine can be administered to relax the smooth muscles of the bladder, reducing bladder spasms and facilitating the surgical procedure.
Management of Chronic Pain
Chronic pain is a complex condition that often requires a multimodal treatment approach. Parasympathetic nerve blockers can play a role in pain management by reducing excessive nerve activity, dampening pain signals, and improving overall quality of life. Nevertheless, it is crucial to consult with a pain specialist or healthcare provider to determine the appropriateness of parasympathetic nerve blockers in an individualized pain management plan.
In the field of palliative care, parasympathetic nerve blockers like scopolamine patches can be used to alleviate symptoms such as excessive saliva production or respiratory secretions in patients with advanced cancer. These medications can provide relief and improve comfort in the final stages of life.
In the management of neuropathic pain, parasympathetic nerve blockers such as glycopyrrolate or ipratropium bromide can be used to reduce nerve-related pain by inhibiting the release of acetylcholine, a neurotransmitter involved in pain signaling.
It is important to note that while parasympathetic nerve blockers can be effective in managing chronic pain, they should be used judiciously and under the guidance of a healthcare professional. These medications may have side effects such as dry mouth, blurred vision, or constipation, which need to be carefully monitored and managed.
In conclusion, parasympathetic nerve blockers have a wide range of clinical applications, from facilitating surgical procedures to managing chronic pain. These medications, when used appropriately and under the guidance of healthcare professionals, can significantly improve patient outcomes and quality of life.
Potential Side Effects and Risks
As with any medication, parasympathetic nerve blockers carry the potential for side effects and risks. While most individuals tolerate these medications well, it is important to be aware of potential adverse effects.
Parasympathetic nerve blockers, also known as anticholinergic medications, work by blocking the action of the parasympathetic nervous system. This system is responsible for regulating various bodily functions, such as digestion, urination, and salivation. By inhibiting the parasympathetic response, these medications can provide relief for certain conditions, but they can also lead to unwanted side effects.
Common Side Effects
Some common side effects associated with parasympathetic nerve blockers include dry mouth, constipation, blurred vision, and urinary retention. These effects arise due to the medications’ interference with the normal parasympathetic functions.
Dry mouth, also known as xerostomia, occurs when the salivary glands do not produce enough saliva. This can cause discomfort, difficulty swallowing, and an increased risk of dental problems. Constipation, on the other hand, is characterized by infrequent bowel movements and difficulty passing stool. It can lead to abdominal pain, bloating, and a general feeling of discomfort.
Blurred vision is another potential side effect of parasympathetic nerve blockers. This occurs because these medications can affect the muscles that control the size of the pupil and the shape of the lens in the eye. As a result, the clarity of vision may be compromised.
Urinary retention, or the inability to fully empty the bladder, can also occur with the use of these medications. This can lead to frequent urination, a weak urine stream, and a feeling of incomplete bladder emptying.
It is crucial to inform your healthcare provider if you experience any concerning symptoms during treatment, as they can provide guidance and support. They may be able to adjust the dosage or recommend additional measures to alleviate these side effects.
Serious Complications
In rare instances, the use of parasympathetic nerve blockers can result in serious complications. These may include severe allergic reactions, cardiovascular disturbances, or adverse effects in specific patient populations.
Severe allergic reactions, known as anaphylaxis, can occur in response to certain medications. Symptoms may include difficulty breathing, swelling of the face or throat, hives, and a rapid heartbeat. If you experience any of these symptoms, it is imperative to seek immediate medical attention.
Cardiovascular disturbances, such as changes in heart rate or blood pressure, can also occur with the use of parasympathetic nerve blockers. These medications can affect the balance between the sympathetic and parasympathetic nervous systems, which regulate heart function. It is important to monitor your heart rate and blood pressure regularly while taking these medications, especially if you have a pre-existing cardiovascular condition.
Furthermore, certain patient populations may be more susceptible to adverse effects from parasympathetic nerve blockers. For example, older adults may be at a higher risk of experiencing cognitive impairment or confusion. Individuals with certain medical conditions, such as glaucoma or urinary obstruction, may also be more prone to complications.
It is imperative to seek immediate medical attention if any unusual or severe reactions occur, and always follow the guidance of a healthcare professional. They can assess your individual risk factors and provide personalized recommendations to ensure your safety and well-being.
Future Perspectives in Parasympathetic Nerve Blocker Research
The field of parasympathetic nerve blockers continues to evolve and present intriguing possibilities for the future. Ongoing research aims to enhance our understanding of these medications and explore their potential in novel therapeutic applications.
Advances in Drug Development
Researchers are actively investigating new drug targets and developing innovative formulations to improve the efficacy and safety of parasympathetic nerve blockers. By refining the pharmacological profiles of these medications, scientists strive to optimize treatment outcomes and minimize potential side effects.
One area of focus in drug development is the exploration of selective parasympathetic nerve blockers. These medications are designed to specifically target certain receptors in the parasympathetic division of the peripheral nervous system, allowing for more precise modulation of parasympathetic activity. This targeted approach may offer advantages in terms of efficacy and side effect profiles, as it avoids unnecessary interference with other bodily functions.
Another avenue of research in drug development involves the investigation of combination therapies. Scientists are exploring the potential synergistic effects of combining parasympathetic nerve blockers with other medications or treatment modalities. By combining different therapeutic approaches, researchers hope to enhance the overall effectiveness of treatment and potentially reduce the dosage required for optimal outcomes.
Potential New Therapeutic Applications
Exciting prospects exist for expanding the clinical applications of parasympathetic nerve blockers. Preliminary studies suggest their potential use in neurological conditions, such as migraine headaches and neurodegenerative diseases. However, more research is necessary to establish their effectiveness and safety in these areas.
In the realm of migraine headaches, parasympathetic nerve blockers have shown promise in reducing the frequency and severity of attacks. By targeting the parasympathetic activity associated with migraines, these medications may provide relief for individuals who suffer from this debilitating condition. Additionally, research is underway to explore the potential of parasympathetic nerve blockers in managing neurodegenerative diseases, such as Alzheimer’s and Parkinson’s. These conditions involve complex disruptions in the nervous system, and parasympathetic modulation may offer a novel approach to mitigating their progression.
Furthermore, parasympathetic nerve blockers are being investigated for their potential role in managing gastrointestinal disorders. The parasympathetic division of the peripheral nervous system plays a crucial role in regulating digestive processes, and dysregulation of parasympathetic activity can contribute to conditions such as irritable bowel syndrome. By modulating parasympathetic activity, these medications may offer relief for individuals suffering from gastrointestinal symptoms.
In conclusion, parasympathetic nerve blockers play a vital role in managing various health conditions by modulating the parasympathetic division of the peripheral nervous system. Understanding their mechanism of action, clinical applications, potential side effects, and ongoing research is crucial for healthcare professionals and patients alike. As with any medication, consulting with a knowledgeable healthcare provider is essential to ensure safe and effective use tailored to individual needs. By staying informed and working hand-in-hand with healthcare professionals, we can navigate the complexities of parasympathetic nerve blockers and harness their therapeutic potential to improve patient outcomes.